Perioperative Blood Transfusion is Associated with the Development of New HLA Antibodies After Adult Lung Transplantation
A. Hicks1, A. Stoker2, M. Cooter2, A. Ali3, J. Klapper4, J. Poisson5, D. Chen5, J. Haney4, K. Ghadimi2, M. Hartwig4, I. Welsby2, B. Bottiger2
1Anesthesiology, Duke University Hospital, South Portland, ME, 2Anesthesiology, Duke University Hospital, Durham, NC, 3Pulmonology, Allergy and Critical Care Medicine, Duke University Hospital, Durham, NC, 4Cardiothoracic Surgery, Duke University Hospital, Durham, NC, 5Pathology, Duke University Hospital, Durham, NC
Meeting: 2021 American Transplant Congress
Abstract number: 96
Keywords: Alloantibodies, Blood transfusion, Lung transplantation, Post-operative complications
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: How to Expect the Unexpected- Incorporating Predictors into Lung Transplant Decision Making
Session Type: Rapid Fire Oral Abstract
Date: Saturday, June 5, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:25pm-6:30pm
Presentation Time: 6:25pm-6:30pm
Location: Virtual
*Purpose: Lung transplant (LT) recipients who develop new antibodies to human leukocyte antigen (HLA) have associated with chronic lung allograft dysfunction and worsened outcomes. We hypothesized that perioperative transfusion is associated with new HLA antibody formation in the first post-operative year after LT.
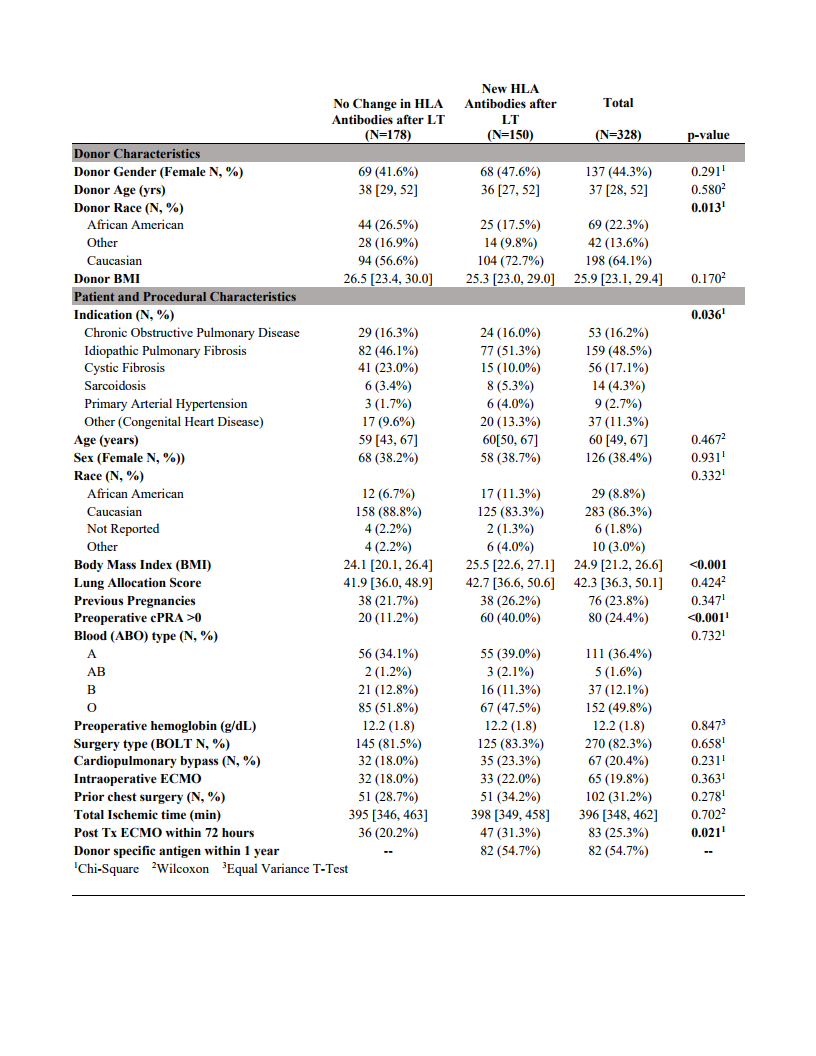
*Methods: In this single center retrospective cohort study, patients undergoing LT from September 2014 to June 2019 were included. Patients requiring multi-organ, redo LT, pre-operative extracorporeal membrane oxygenation support, or preoperative calculated panel reactive antibody screen >50% were excluded. Patient and procedural characteristics, blood products transfused within 72 hours, and HLA antibody profiles were abstracted from the medical record. The primary outcome was formation of new HLA antibodies within 12 months of transplant. Patients were grouped into those that developed new HLA antibodies (“new HLA”) or those that did not change their HLA antibody profiles (“no change”) and compared. Secondary outcomes included severe primary graft dysfunction (PGD grade 3), severe acute kidney injury by KDIGO (AKI). These are described by univariate analysis.
*Results: Three hundred and twenty-eight patients were included, with 178 in the unchanged group and 150 in the new HLA group. Recipients in the new HLA group had more Caucasian donors, higher baseline cPRAs, different indications for transplant, slightly higher body mass indices, and more postoperative ECMO (Figure). Compared to the no change group, the new HLA group received more plasma (FFP; 1 [0,3] vs 0 [0,1], p<0.001), and cryoprecipitate (0 [0,2] vs 0 [0,1], p=0.003), while median units of red blood cells and platelets transfused were not statistically different. Total numbers of units transfused were significantly higher in the group with new HLA antibodies (4 [2, 12] vs 3 [1, 6], p=0.007). Patients in the new HLA group had a higher incidence of severe PGD (25% v 15%, p=0.015) and severe AKI (20% v 10%, p=0.019) compared to those in the no change group.
*Conclusions: In lung transplant recipients, perioperative transfusion is associated with development of new HLA antibodies within the first year. Newly positive patients had a higher associated incidence of severe PGD and severe AKI.
To cite this abstract in AMA style:
Hicks A, Stoker A, Cooter M, Ali A, Klapper J, Poisson J, Chen D, Haney J, Ghadimi K, Hartwig M, Welsby I, Bottiger B. Perioperative Blood Transfusion is Associated with the Development of New HLA Antibodies After Adult Lung Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/perioperative-blood-transfusion-is-associated-with-the-development-of-new-hla-antibodies-after-adult-lung-transplantation/. Accessed July 18, 2025.« Back to 2021 American Transplant Congress