Oxalate Nephropathy After Kidney Transplant: Defining Histological Patterns, Contributing Factors and Graft Outcome
1Nephrology, Mayo Clinic, Scottsdale, AZ, 2Nephrology, Mayo Clinic, Rochester, MN, 3Nephrology, Mayo Clinic, Jacksonville, FL
Meeting: 2021 American Transplant Congress
Abstract number: 174
Keywords: Graft failure, Kidney, Nephropathy, Outcome
Topic: Clinical Science » Kidney » Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:05pm-6:10pm
Presentation Time: 6:05pm-6:10pm
Location: Virtual
*Purpose: The objective of this study is to evaluate KTx recipients with biopsy proven oxalate nephropathy (ON) to better define risk factors, histologic patterns and graft outcome in patients without primary hyperoxaluria (PH).
*Methods: All renal allograft biopsy reports from 2008 to 2018 at the three Mayo transplant centers (Arizona, Florida, Minnesota) were queried for pathologist diagnosis of ON and verified by chart review. All patients with PH diagnosis were excluded. Risk factors for enteric causes for ON, histological findings, serum and urine oxalate levels around time of biopsy, treatment, and allograft outcomes were analyzed.
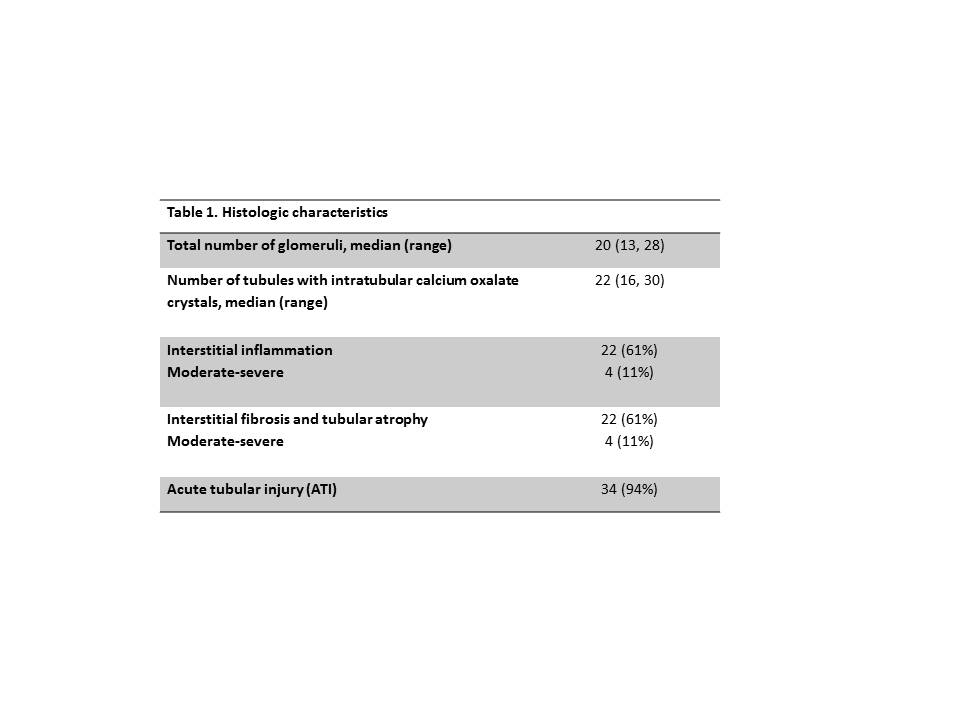
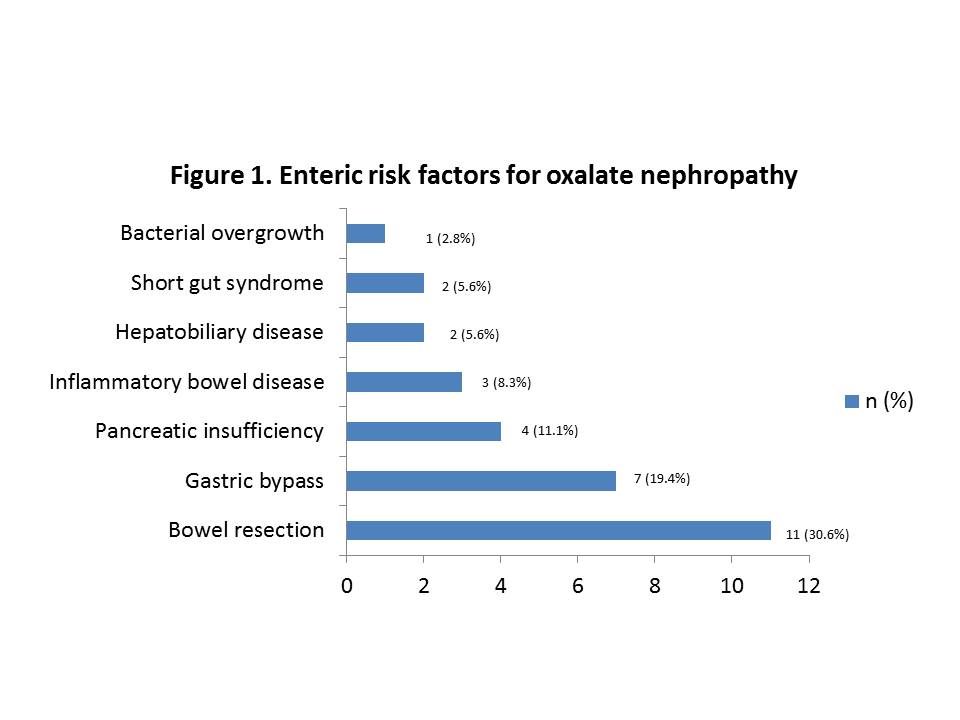
*Results: 36 patients were identified. Mean age at diagnosis of ON was 57.5 years, 50% were female, 83.3% white, 88.9% first KTx, and 36% were pre-emptive to Tx. Most common cause of ESRD was diabetes (36%), and 11.1% due to enteric oxalosis. 17% had pre-KTx history of kidney stones. Median baseline GFR was 43.8ml/min. Median time from KTx to ON diagnosis was 6.9 months (range 1.25-47 months). Diarrhea was the most prevalent risk factor in 42% of patients. Enteric disorders were identified in 83% of patients as shown in Figure 1. 61% of patients had stage II or III acute kidney injury (AKI) and 55.6% required dialysis at the time of biopsy. Plasma oxalate (median 15.7micromol/L, n=25), and urine oxalate (median 58.1mg/24hr, n=21) were elevated. Histological findings are described in table 1. Management included low oxalate diet education (64%), calcium supplementation with food (61%), pyridoxine (14%), and steroid treatment (81%). After a median follow-up of 33.5 months, median eGFR was 27.7ml/min, with 53% of patient with eGFR<30ml/min.
*Conclusions: This is the largest case series of ON after KTx showing that enteric causes account for 83% of cases and chronic diarrhea is a common risk factor. Severe AKI and acute tubular injury are common. Despite low rates of severe inflammation or IFTA, there was a significant drop in GFR from baseline to last follow-up. Further studies need to define histologic characteristics linked with adverse outcomes.
To cite this abstract in AMA style:
Jakob N, Chuu A, Ninan J, Lim E, Zhang N, Amer H, Cosio F, Wadei H, Ryan M, Cortese C, Cornell L, Keddis M. Oxalate Nephropathy After Kidney Transplant: Defining Histological Patterns, Contributing Factors and Graft Outcome [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/oxalate-nephropathy-after-kidney-transplant-defining-histological-patterns-contributing-factors-and-graft-outcome/. Accessed March 7, 2026.« Back to 2021 American Transplant Congress