Outcomes of Primary Kidney Transplant Recipients with Human Immunodeficiency Virus According to Induction Immunosuppression in the United States
1MEDICINE, University of Minnesota, Minneapolis, MN, 2Analytics, MHealth-Fairview, Minneapolis, MN, 3Medicine, University of Minnesota, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 1377
Keywords: Graft survival, HIV virus, Induction therapy, Outcome
Topic: Clinical Science » Kidney » 37 - Kidney Immunosuppression: Induction Therapy
Session Information
Session Name: Kidney Immunosuppression: Induction Therapy
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Hall C
*Purpose: Early reports of outcomes in recipients with HIV suggested lower kidney rejection rate in association with depletional induction. However, these reports did not assess long-term recipient and graft survival.
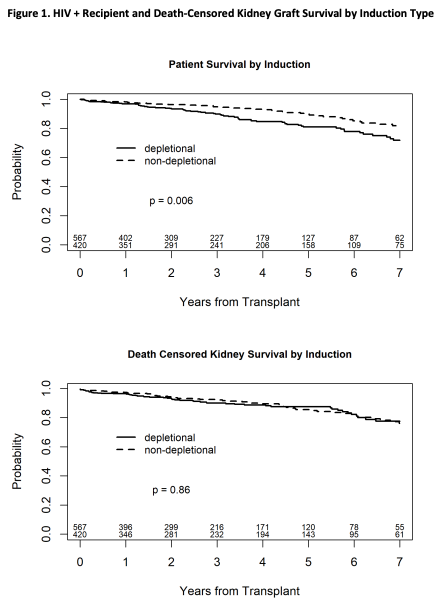
*Methods: We analyzed the Scientific Registry of Transplant Recipients (SRTR) standard analysis file for all HIV positive primary kidney transplant recipients between 01/01/2004 and 12/2/2020. We excluded those with mixed induction regimen, steroid-only induction, or missing induction data. All recipients were discharged on maintenance immunosuppression with tacrolimus and mycophenolate with or without steroids (N=987). Recipients were grouped according to the type of induction received: a depletional group (n=567) and a non-depletional group (n=420). Kaplan-Meier curves were generated to examine recipient and graft survival by induction type. Follow up time was censored at seven years post-transplant. We used Cox proportional hazard models to examine the association between induction type and outcomes of interest. Models were further adjusted for recipient age and sex, PRA, HCV co-infection, donor type, dialysis vintage, donor type and age, primary payor, transplant year and steroid maintenance. Transplant center was included as a random effect.
*Results: Rejection rates by one-year post transplant were observed in a 12.6% in the depletional group and a 12.8% in the non-depletional group (P-value >0.999). Similarly, DGF rate, re-hospitalizations, and the 1-year creatinine did not differ statistically between groups. In the Kaplan-Meier analysis, recipients of non-depletional induction had better survival (log-rank P=0.006). Death-censored kidney graft survival did not differ by induction type (log-rank p=0.86) (Figure-1). In the multivariable analysis, compared to depletional induction, non-depletional induction was associated with 41.5% improved recipient survival (LLCI, aHR, ULCI) (0.39, 0.585, 0.88). Death-censored graft survival was not statistically different between induction groups (0.66, 0.99, 1.48).
*Conclusions: In the settings of tacrolimus and mycophenolate maintenance immunosuppression, primary kidney transplant recipients with HIV appear to have better survival in association with non-depletional induction up to seven years post-transplant.
To cite this abstract in AMA style:
Bhunia K, Swanson K, Bregman A, El-Rifai R, Spong R, Jackson S, Riad S. Outcomes of Primary Kidney Transplant Recipients with Human Immunodeficiency Virus According to Induction Immunosuppression in the United States [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-primary-kidney-transplant-recipients-with-human-immunodeficiency-virus-according-to-induction-immunosuppression-in-the-united-states/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress