Outcomes of Living and Deceased Donor Liver Transplant Recipients According to the MELD Score
J. Lee, J. Lee, D. Joo, D. Han, M. Ju, J. Choi, S. Kim, M. Kim.
Department of Surgery, Yonsei University College of Medicine, Seoul, Republic of Korea.
Meeting: 2015 American Transplant Congress
Abstract number: C122
Keywords: Allocation, Liver transplantation, Living-related liver donors, Survival
Session Information
Session Name: Poster Session C: Liver Donation and Allocation
Session Type: Poster Session
Date: Monday, May 4, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background
Living donor liver transplantation (LDLT) has developed as an alternative to decease donor liver transplantation (DDLT) to overcome the critical shortage of deceased organ donations. However, the evidence supporting a LDLT for high model for end stage liver disease (MELD) score recipient is weak. We compared the outcomes of LDLT and DDLT according to MELD scores.
Methods
The study included 425 adult patients who underwent liver transplantation between 2006 and 2013 at Severance Hospital (268 LDLT, 157 DDLT). Patients with re-transplantation and fulminant liver failure were excluded from the study. Recipients were categorized according to their MELD score into low (MELD score ≤25) and high (MELD score >25) MELD group.
Results
Recipient characteristics were similar between LDLT and DDLT, with the exception of higher MELD score in DDLT group (19.85 vs. 13.52, p<0.001). The DDLT donors were significantly older than LDLT donors (42.55 vs. 31.48, p<0.001). Hepatocellular carcinomas were present in 57.4% of the recipients (60.8% in LDLT vs. 51.6% in DDLT, p=0.063). The median follow-up was 32 months (range, 0 to 105 months). LDLT demonstrated significantly better patient survival than DDLT in low MELD group (86.9% vs. 74.8% at 5 years, p=0.006). Survival after LDLT was not inferior to DDLT in high MELD group (72.1% vs. 57.3% at 5 years, p=0.265).
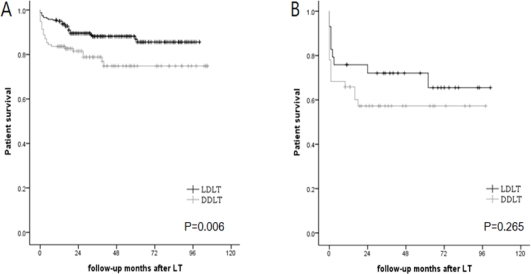 Patient survival by time since LDLT or DDLT for (A) patients with a MELD score ≤ 25 and (B) patients with a MELD score > 25
Patient survival by time since LDLT or DDLT for (A) patients with a MELD score ≤ 25 and (B) patients with a MELD score > 25
LDLT=living donor liver transplantation, DDLT=deceased donor liver transplantation, MELD=model for end stage liver disease
Conclusion
LDLT provided similar survival to DDLT in high MELD score recipients. Thus, when deceased donor organs are scare, a high MELD score should not be a contraindication to LDLT.
To cite this abstract in AMA style:
Lee J, Lee J, Joo D, Han D, Ju M, Choi J, Kim S, Kim M. Outcomes of Living and Deceased Donor Liver Transplant Recipients According to the MELD Score [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-living-and-deceased-donor-liver-transplant-recipients-according-to-the-meld-score/. Accessed July 15, 2025.« Back to 2015 American Transplant Congress
