Outcomes of Kidney Transplant Recipients With Sickle Cell Disease: An Analysis of the 2000-2019 UNOS/OPTN Database
1Saint Luke's Health System, Kansas City, MO, 2Mayo Clinic, Rochester, MN, 3Mayo Clinic, Phoenix, AZ, 4Mount Auburn Hospital, Cambridge, MA, 5University of Pittsburgh Medical Center Pinnacle, Harrisburg, PA, 6University of Mississippi Medical Center, Jackson, MS, 7Medstar Georgetown Transplant Institute, Washington, DC
Meeting: 2021 American Transplant Congress
Abstract number: 177
Keywords: Graft failure, Kidney transplantation, Outcome, Survival
Topic: Clinical Science » Kidney » Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:20pm-6:25pm
Presentation Time: 6:20pm-6:25pm
Location: Virtual
*Purpose: Lower patient survival has been observed in sickle cell disease (SCD) patients who go on to receive a kidney transplant. This study aimed to assess the post-transplant outcomes of SCD kidney transplant recipients in the contemporary era.
*Methods: We used the OPTN/UNOS database to identify first-time kidney transplant recipients from 2010 through 2019. We compared patient and allograft survival between recipients with SCD vs. all other diagnoses (non-SCD) as the reported cause of end-stage kidney disease. We examined whether post-transplant outcomes improved among SCD in the recent era (2010-2019), compared to the early era (2000-2009).
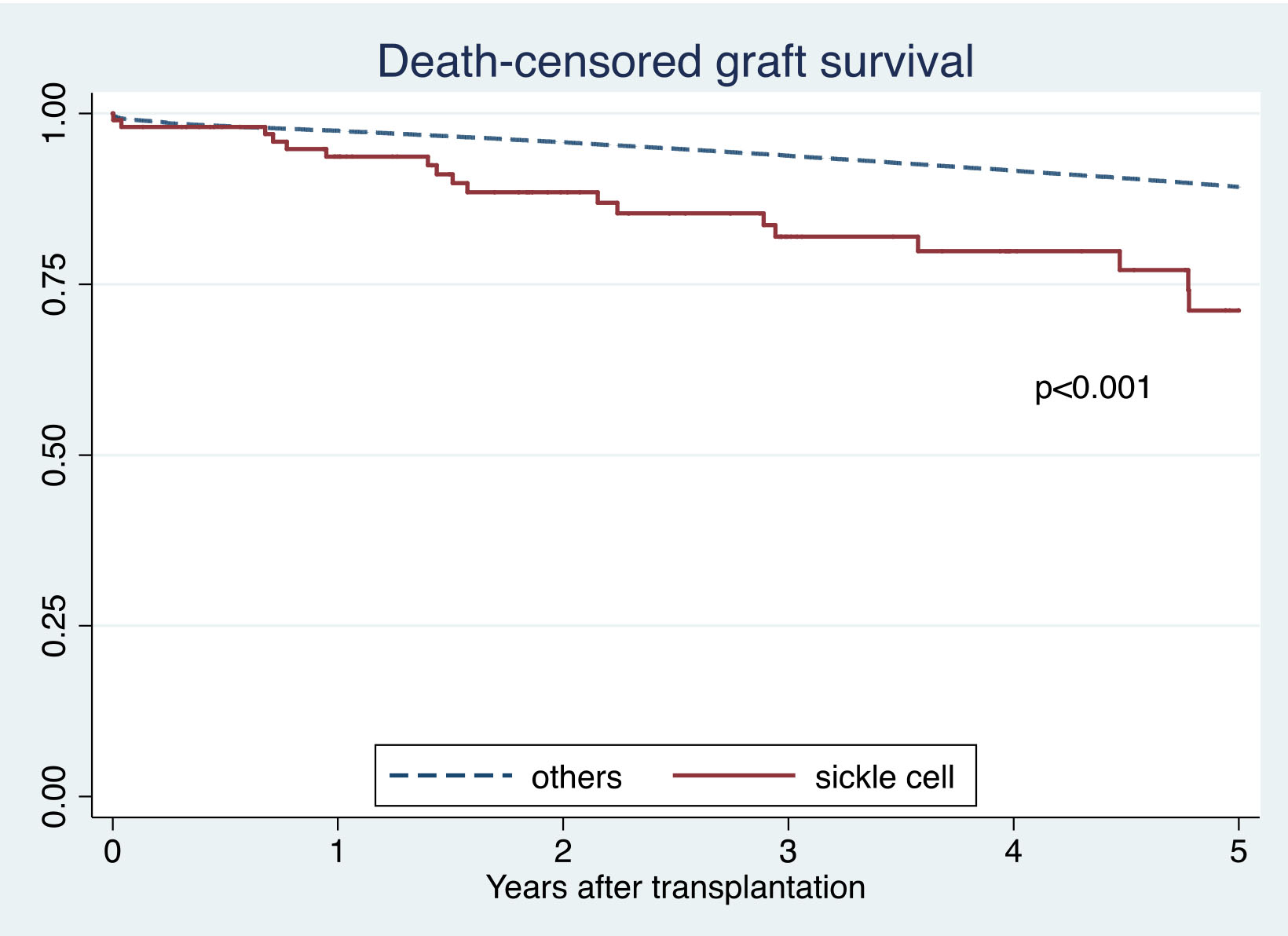
*Results: This study included 105 SCD and 146,325 non-SCD kidney transplant recipients. SCD recipients were younger, more likely to be female, African-American, and have a lower body mass index. They were more likely to have a higher panel reactive antibody and be on dialysis at the time of transplant. Five-year death-censored graft survival in SCD was lower than non-SCD recipients (71% vs. 89%; p<0.001), whereas five-year patient survival was comparable between two groups (83% vs. 87%; p=0.12). After adjusting for differences in baseline characteristics, SCD was significantly associated with lower patient survival (HR 2.87; 95% CI 1.75-4.68, p<0.001) and death-censored graft survival (HR 1.98; 95% CI 1.30-3.01, p=0.001), compared to non-SCD recipients. When we further investigated outcomes, compared to recipients with diabetes mellitus, hypertension, and glomerular disease as a cause for their end-stage kidney disease, SCD was significantly associated with lower patient survival and death-censored graft survival. There were no differences in patient survival (p=0.61), and death-censored graft survival (p=0.38) of SCD recipients in the recent and early era.
*Conclusions: Patient and allograft survival in SCD kidney recipients were worse than recipients with other diagnoses. The outcomes of SCD in the recent era did not improve from the early era. Thus, there is an urgent need for scientific research on interventions to improve post-transplant outcomes of SCD kidney transplant recipients.
To cite this abstract in AMA style:
Leeaphorn N, Thongprayoon C, Jadlowiec C, Chewcharat A, Hansrivijit P, Katari S, Vaitla P, Cummings L, Cooper M, Cheungpasitporn W. Outcomes of Kidney Transplant Recipients With Sickle Cell Disease: An Analysis of the 2000-2019 UNOS/OPTN Database [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-kidney-transplant-recipients-with-sickle-cell-disease-an-analysis-of-the-2000-2019-unos-optn-database/. Accessed February 24, 2026.« Back to 2021 American Transplant Congress