Outcomes Following Deceased Donor Split/Partial Liver Transplant for Hepatocellular Carcinoma
Vanderbilt University Medical Center, Nashville, TN
Meeting: 2020 American Transplant Congress
Abstract number: A-137
Keywords: Graft survival, Malignancy, Split-liver transplantation
Session Information
Session Name: Poster Session A: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: To mitigate waiting time for liver transplant for hepatocellular carcinoma (HCC) and increase available organs, partial or split liver transplant (SLT) has been utilized. There was concern, however, that regeneration of these grafts would stimulate cytokines and growth factors, negatively affecting oncologic outcomes. Our study aimed to examine outcomes following deceased donor SLT in comparison to WLT for patients with HCC.
*Methods: A retrospective analysis of Scientific Registry of Transplant Recipients records of adult deceased donor, SLT and WLT recipients with HCC from 2002-2017 was conducted. A 1:1 cohort of WLT recipients was identified through logistic regression-based propensity score matching on characteristics including recipient age, liver donor risk index (LDRI), recipient body mass index, donor and recipient diabetes and laboratory model for end-stage liver disease score (all p<0.05), and stratification to ensure comparability in potential follow-up time and etiology of liver disease. Differences in pre-transplant demographic and clinical characteristics were evaluated using Chi-square tests with z-tests of column proportions or t-tests. Kaplan-Meier and multivariable Cox proportional hazards regression models evaluated the main and co-variable-adjusted effects of SLT on survival.
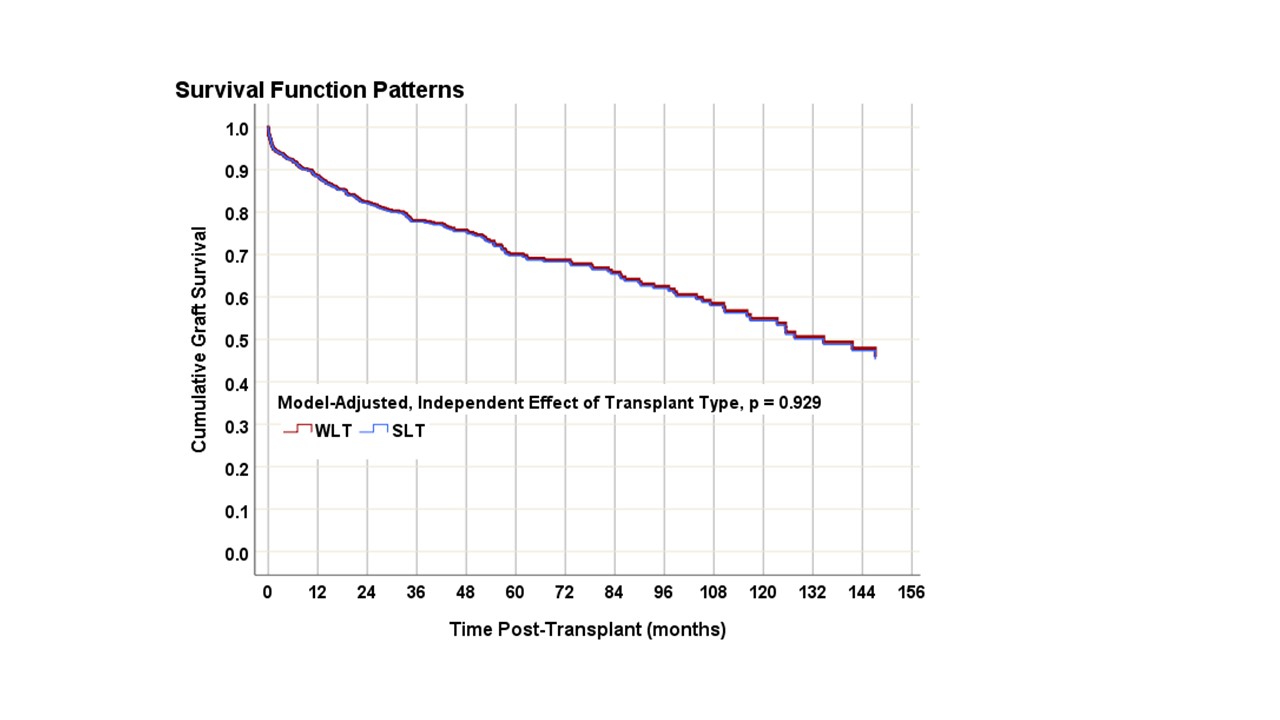
*Results: The sample included 330 adults with HCC who underwent SLT and a matched cohort of 330 patients with HCC who underwent WLT. Despite statistical incorporation in propensity scores, SLT patients had higher mean LDRI scores (1.9±0.29 vs. 1.5±0.42, p<0.001), and a higher proportion were female (43% vs. 26%, p<0.001) and of normal or healthy weight (41% vs. 25%, p<0.001). Donors for the SLT cohort had higher proportions with normal or healthy weight (58% vs 35%, p<0.001) and lower rates of diabetes (2% vs 12%, p<0.001). Graft survival averaged (95%CI) 112 (103, 121) and 107 (98, 116) months for SLT and WLT, respectively. After adjusting for clinical and demographic risk factors, there were no differences in graft or patient survival between cohorts (both p≥0.929) (Figure 1).
*Conclusions: This is the first large database study performed using matched cohorts and reports equivalent outcomes in patients with HCC undergoing deceased donor SLT compared to WLT. SLT was not an independent risk factor for graft loss. Further studies need to be performed to further elucidate differences in these populations to determine the “right” candidate for SLT.
To cite this abstract in AMA style:
Matsuoka L, Sutcliffe T, Feurer I, Rega S, Alexopoulos S. Outcomes Following Deceased Donor Split/Partial Liver Transplant for Hepatocellular Carcinoma [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-following-deceased-donor-split-partial-liver-transplant-for-hepatocellular-carcinoma/. Accessed February 20, 2026.« Back to 2020 American Transplant Congress