Osmotic Demyelination Syndrome after Liver Transplantation- Etiology and Treatment Options
1Indiana Univ School of Medicine, Pavia University School of Medicine, Indianapolis, IN, 2Indiana Univ School of Medicine, Indianapolis, IN
Meeting: 2019 American Transplant Congress
Abstract number: B323
Keywords: Liver transplantation, Plasmapheresis, Post-operative complications, Prognosis
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Orthotopic liver transplantation (OLT) is the only effective therapy for patients with end stage liver failure that increases long-term survival, but is not without complications. One rare and devastating complication is osmotic demyelination syndrome (ODS). The purpose of this study is to evaluate the plasmapheresis (PLEX) as a treatment option in patients with ODS after liver transplantation.
*Methods: Charts for all patients undergoing OLT at our center between January 2007 and March 2017 (n=1140) were retrospectively reviewed. From this data, 146 patients underwent neurological work up for postoperative neurological changes.
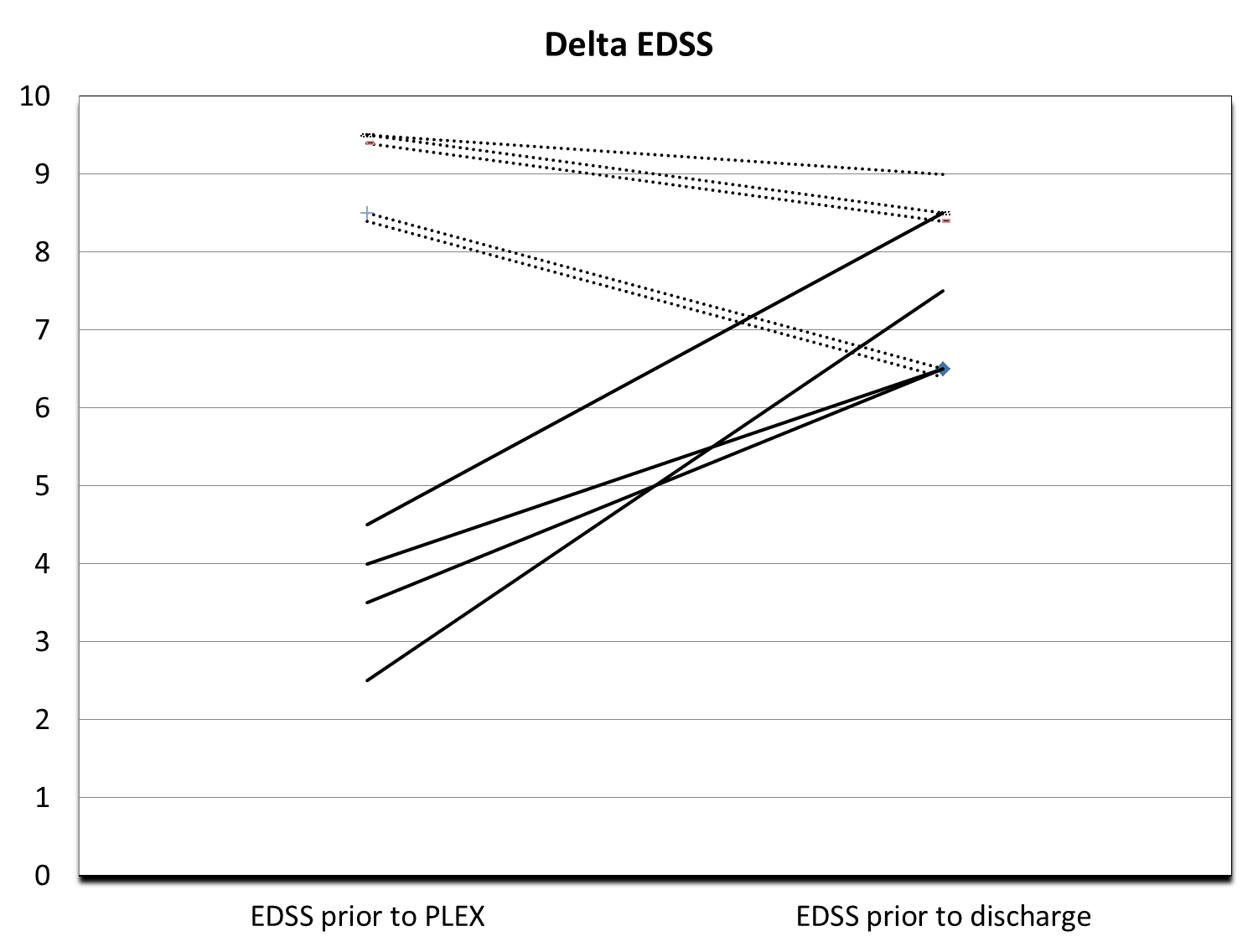
*Results: Of these, nine patients were diagnosed with ODS based on clinical symptoms and brain MRI findings. The leading indication for neurological consultation was altered mental status. Other symptoms included: dysarthria, dysphagia, difficulty with tongue movements, increased tone, weakness of extremities, tremor, myoclonus, ataxia, pseudobulbar affect, frontal release signs, hallucinations, and seizures. Five of these nine patients were treated with plasmapheresis and none received intravenous immunoglobulin. Neurological evaluation was done with MRI head, EEG and Kurtzke’s Expanded Disability Status Scale (EDSS) score prior to discharge and upon follow-up. The median follow up was 465 days. Data gathered from the electronic medical record included age at time of OLT, gender, indication for OLT, diagnosis of alcoholic cirrhosis, presence of pre-transplant encephalopathy, operative time, blood loss during operation, amount of blood product and IVF transfusion, requirement of postoperative dialysis or continuous veno-venous hemodialysis (CVVH), pre-transplant sodium level, post-transplant sodium level, other electrolyte fluctuations within 48 hours of the postoperative period, and tacrolimus peak levels within the first fourteen days of surgery. All analyzes has been done by non-parametric analysis. The only predictor for ODS is the intraoperative blood loss (Tab 1). The plasmapheresis group had significantly better EDSS score and their EDSS score had improved significantly during the hospital stay (Fig 1).
*Conclusions: ODS is a rare and potentially devastating complication after OLT. It requires a high degree of clinical suspicion. It is important to monitor several factors in patients undergoing liver transplant, these include pre-operative and post-operative sodium levels as well as administration of blood products. The only valid treatment is early plasmapheresis, which have been shown to improve the patient’s neurological status and outcomes.
| Factor | p-value |
| Operative time | 0.364 |
| Blood loss | 0.047 |
| Delta sodium | 0.117 |
| Delta chloride | 0.118 |
| Tacrolimus peak | 0.897 |
| Pre-transplant phosphorus level | 0.064 |
| Age at time of OLT | 0.068 |
To cite this abstract in AMA style:
Mihaylov P, Soma D, Kuruppu D, Ekser B, Mangus R, Fridell J, Snook R, Kubal C. Osmotic Demyelination Syndrome after Liver Transplantation- Etiology and Treatment Options [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/osmotic-demyelination-syndrome-after-liver-transplantation-etiology-and-treatment-options/. Accessed February 26, 2026.« Back to 2019 American Transplant Congress