Organ Care System Use in Liver Transplantation Shifts Preservation-Reperfusion Injury in Time and Space
Department of Transplant Pathology, University of Pittsburgh, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 441
Keywords: Liver, Liver preservation, Perfusion, Preservation
Topic: Clinical Science » Organ Inclusive » 69 - Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Information
Session Name: Surgical Issues: Donor and Recipient
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:20pm-4:30pm
Presentation Time: 4:20pm-4:30pm
Location: Hynes Room 310
*Purpose: Liver allograft ischemia-reperfusion injury (IRI) causes early allograft dysfunction (EAD). The TransMedics Organ Care System (OCS) PROTECT trial for liver transplantation (NCT02522871) revealed that both brain death (DBD) and circulatory death (DCD) donors, when OCS-preserved, experienced a lower incidence of EAD compared to standard of care (SOC). This study explores histological and pathophysiological reasons for the differences.
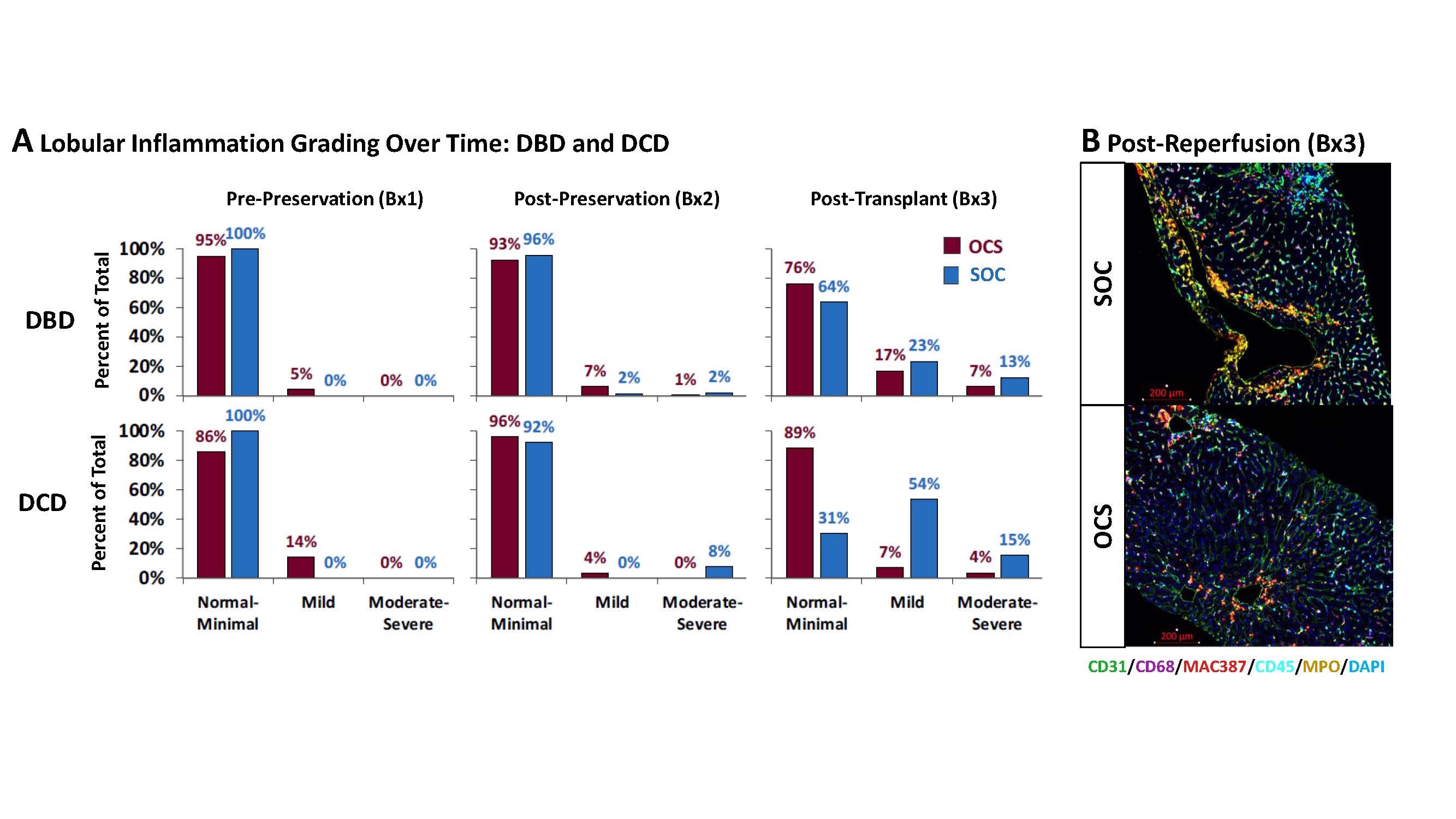
*Methods: Biopsies obtained pre-retrieval from the donor (Bx1), post-preservation (Bx2), and after reperfusion in the recipient (Bx3) were scored for histopathological parameters of IRI by a central pathologist without knowledge of preservation method or donor organ type.
*Results: At Bx1, most (91%) OCS (n=150) and SOC (n=139) biopsies exhibited none to mild histological changes for lobular necrosis and inflammation, indicating effective randomization. In Bx2, OCS showed slightly increased inflammation and necrosis in OCS vs SOC (Panel A, composite score, p=0.22) indicating some degree of IRI in the former, whereas the latter were frozen in time due to cold static storage. Throughout the preservation process (Bx 1 vs. Bx 3), lobular inflammation severity was significantly less in OCS and SOC (p=0.003), 36% of SOC livers had mild/moderate worsening vs. 15% of OCS. This indicates that OCS ameliorated manifestations of IRI in the recipient by normothermic extracorporeal perfusion. The difference in lobular necrosis and inflammation between OCS and SOC was most significant in DCD organs (n=27 vs. 13, composite score, p=0.03). Three livers turned down for use all had peculiar abnormalities present at Bx 1 indicative of damage while in the donor and not on the machine and rendered recognizable by OCS perfusion. Preliminary multiplex immunohistochemistry (Panel B) reveals an increase in innate immune cells [MPO+ neutrophils (gold), recent monocyte immigrants (MAC387+; red), and CD68+ macrophages (purple)] in Bx 3 in SOC vs. OCS-preserved organs suggestive of less innate immunity activation after transplantation.
*Conclusions: IRI is occurs regardless of preservation method. SOC-preserved organs are “frozen in time and space” for Bx1 and Bx2; afterward the entire IRI process unfolds in the recipient contributing to EAD (Bx 3). In contrast, OCS Bx2 enables assessment of IRI and organ function (bile production), ex vivo, enabling proactive identification, monitoring, and responding to IRI ex vivo rather than reacting in vivo after transplant. When placed into the recipient, less significant EAD is detected.
To cite this abstract in AMA style:
Demetris AJ, Wood-Trageser MA, Lesniak D, Investigators -ThePROTECT. Organ Care System Use in Liver Transplantation Shifts Preservation-Reperfusion Injury in Time and Space [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/organ-care-system-use-in-liver-transplantation-shifts-preservation-reperfusion-injury-in-time-and-space/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress