Natural Killer Cell NKG2D Receptor Mediates Airway Cell Hypoxic Injury Through Recognition of Stress Molecules
1University of California, San Francisco, San Francisco, CA, 2Medicine, University of California, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 666
Keywords: Ischemia, Lung transplantation, Natural killer cells
Topic: Basic Science » Basic Science » 14 - Ischemia Reperfusion
Session Information
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Primary graft dysfunction (PGD), the clinical syndrome of pulmonary hypoxia and reperfusion, occurs afer 1/3 of all lung transplants, and accounts for excess mortality. Previously, we showed a novel role of the Natural Killer (NK) cell stress receptor, NKG2D, in mouse models of PGD. We hypothesized that NKG2D stress molecules would be increased on hypoxic human airway cells and recognized by NK cells.
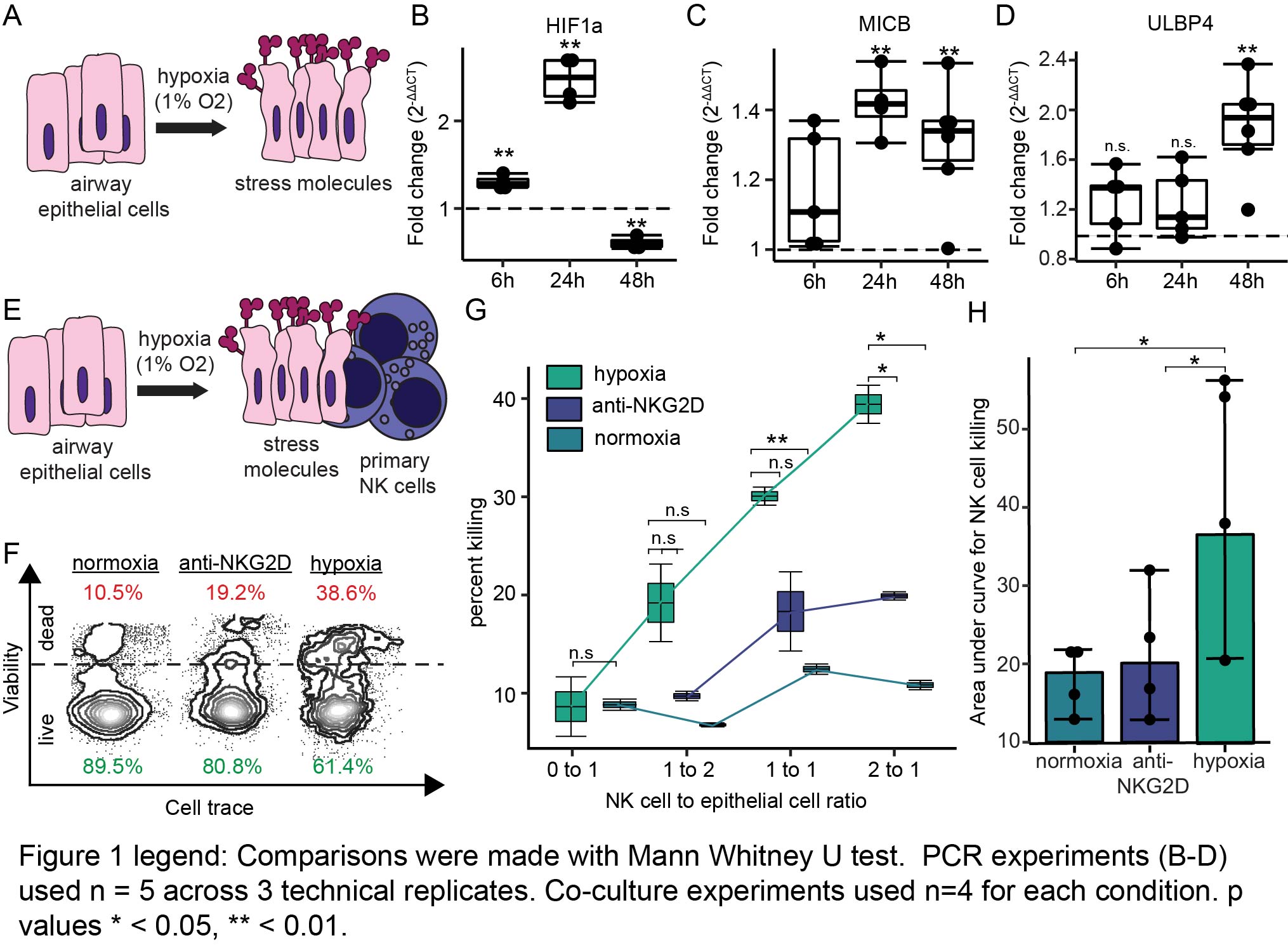
*Methods: Human airway epithelial cells were subjected to 6, 24, or 48 hours of hypoxia (n = 5, 1% oxygen) or normoxia (n = 5, 21% oxygen) (Fig. 1A). We measured transcripts of 8 human stress molecules (MICA, MICB, ULBP1-6) and hypoxia inducible factor 1a (HIF1A) by PCR and quantified fold change. NK cell cytotoxicity (n = 4) of normoxic or hypoxic airway epithelial cells was measured by flow cytometry after 24 hours of co-culture with primary human NK cells. NK cells were also treated with blocking anti-NKG2D monoclonal antibody before co-culture. Comparisons between conditions were made with the Mann Whitney U test.
*Results: HIF1A mRNA (Fig. 1B) was induced at 6 hours (p = 0.004) and 24 hours (p = 0.0001) but decreased at 48 hours (p = 0.001). All 8 human stress molecule transcripts (MICA, MICB, ULBP1-6) were increased within 48 hours of hypoxia. MICB (Fig. 1C) was increased by 1.4-fold (interquartile range [IQR] 1.38-1.46, p = 0.003) at 24 hours and 1.34-fold at 48 hours (IQR 1.26 – 1.37, p = 0.008). ULBP4 was increased 1.94-fold at 48 hours (IQR 1.72-2.1, p = 0.003, Fig. 1D). Figures 1E and 1F depict the design of co-culture experiments and representative flow cytometry cytotoxicity plots. We found that NK cells killed hypoxic epithelial cells at increased rates at any concentration when compared to the normoxia or anti-NKG2D groups (Figs. 1F & 1G). This was most evident at an effector to target ratio of 2:1, with 39% (IQR 38-40) cytotoxicity among hypoxic epithelial cells compared to anti-NKG2D NK cells (20%, IQR 19-20, p = 0.03) and normoxic epithelial cells (11%, IQR 10.8-11.1, p = 0.02). There was significantly increased area under the cytotoxicity curve for hypoxic epithelial cells compared to the normoxia (p = 0.02) or anti-NKG2D (p = 0.04) groups (Fig. 1H).
*Conclusions: Airway epithelial cell stress ligand transcripts are increased in response to hypoxia. Stress molecules are induced in a similar pattern to HIF1A but vary across time. NK cells kill hypoxic epithelial cells in an NKG2D receptor-dependent manner. A monoclonal antibody against the NKG2D receptor shows potential as a therapy for PGD.
To cite this abstract in AMA style:
Tsao T, Aminian E, Shemesh A, Tran L, Wang P, Deiter F, Greenland JR, Calabrese DR. Natural Killer Cell NKG2D Receptor Mediates Airway Cell Hypoxic Injury Through Recognition of Stress Molecules [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/natural-killer-cell-nkg2d-receptor-mediates-airway-cell-hypoxic-injury-through-recognition-of-stress-molecules/. Accessed February 28, 2026.« Back to 2022 American Transplant Congress