Molecular Features of Rejection in Endobronchial Mucosa Biopsies
University of Alberta, Edmonton, AB, Canada
Meeting: 2019 American Transplant Congress
Abstract number: C322
Keywords: Gene expression, Lung transplantation
Session Information
Session Name: Poster Session C: Lung: All Topics
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Mucosal biopsies are safer and easier to collect than transbronchial biopsies (TBB) but cannot be assessed histologically for lung rejection. Reliable assessment would change care by reducing patient risk and permitting biopsies of sicker patients, and provide insights into rejection. We assessed mucosal biopsies from the third bronchial bifurcation (3BMB) with the Molecular Microscope (MMDx).
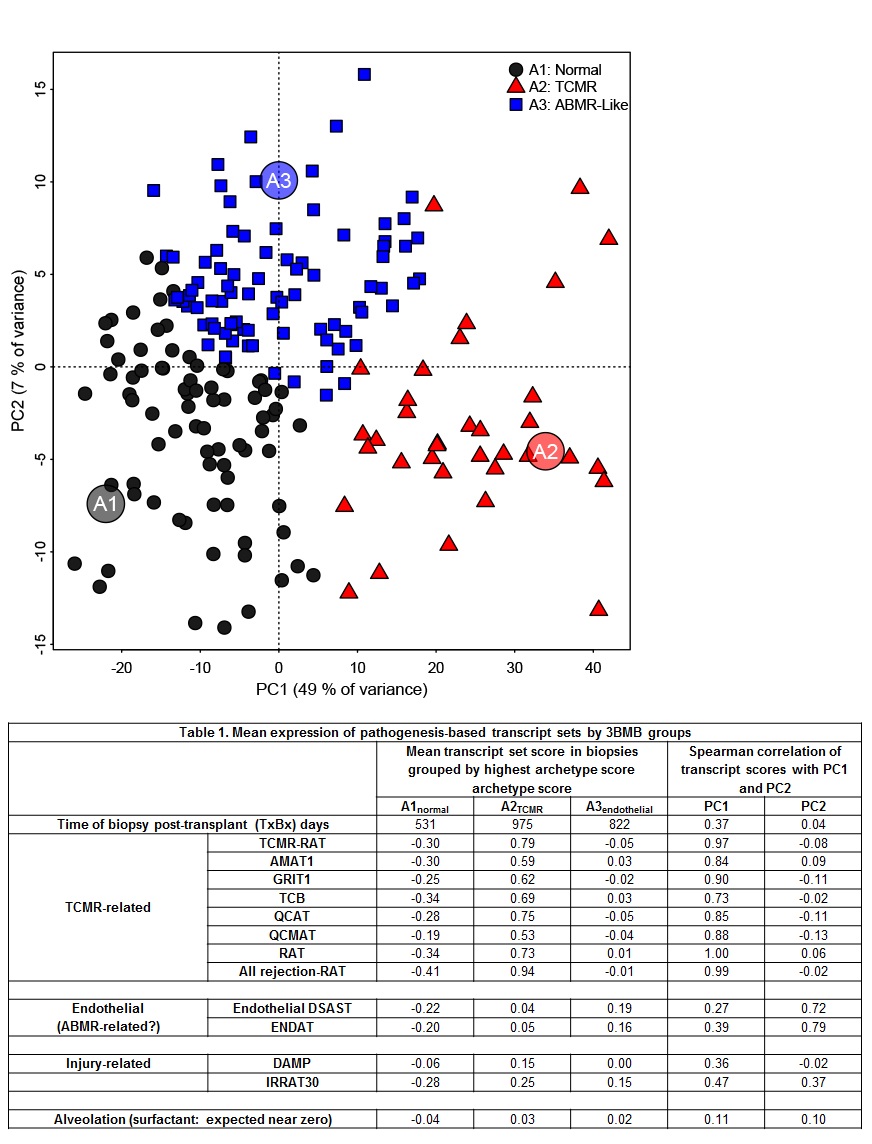
*Methods: 198 single piece 3BMBs from 7 centers in the INTERLUNG study (ClinicalTrials.gov: NCT02812290) were processed on microarrays. We derived 3 scores (S1normal, S2TCMR, S3ABMR-like) with unsupervised machine learning (archetypal analysis, principal component analysis) using rejection-associated transcripts identified in kidneys and validated in hearts. We examined the scores in relation to pathogenesis-based transcripts annotated in rejection & injury of TBBs and other organs because 3BMBs are unclassifiable by histology.
*Results: Machine learning identified 3 archetypes & scored biopsies for similarity to each: relatively normal (S1normal), rejection/TCMR (S2TCMR), and ABMR-like (S3ABMR-like). Low S1normal and high PC1/S2TCMR scores correlated with histologic ISHLT B grade>0 in paired TBBs (i.e. airway lesions; p<0.05), but not A grade (i.e. alveoli). In biopsies grouped by highest archetype score (Table 1) pathogenesis-based transcript set expression reflected rejection/TCMR-like changes in group A2TCMR, with high expression of IFNG-inducible transcripts (GRIT1), effector T cell transcripts (e.g. QCATs) and macrophage transcripts typical of rejection/TCMR in kidneys, hearts, and TBBs. S3ABMR-like correlated with endothelial transcripts elevated in ABMR in other organs, but not DSA, and may not reflect true ABMR given that ABMR was not suspected in most biopsies in this early cohort (median 376 days post-tx). PC1 also primarily correlated with rejection-related changes.
*Conclusions: T cell-mediated rejection-like phenotypes resembling those described in molecular studies of other organs are identifiable by molecular assessment of 3BMBs, correlating with B grade airway lesion histology in the paired TBB for these 3BMBs. Whereas histology requires up to 10 TBBs and cannot assess 3BMBs, molecular assessment of 3BMBs can be informative with very few 3BMB pieces and can potentially be used in patients with respiratory compromise.
To cite this abstract in AMA style:
Parkes MD, Halloran KM, Chang J. Molecular Features of Rejection in Endobronchial Mucosa Biopsies [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/molecular-features-of-rejection-in-endobronchial-mucosa-biopsies/. Accessed March 7, 2026.« Back to 2019 American Transplant Congress