Long-Term Outcomes After Pediatric Liver Transplantation for Malignant Liver Tumors: Effects of Era and Age.
1Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN
2Cincinnati Children's Hospital Medical Center, Cincinnati, OH.
Meeting: 2016 American Transplant Congress
Abstract number: 355
Keywords: Hepatocellular carcinoma, Liver transplantation, Malignancy, Pediatric
Session Information
Session Name: Concurrent Session: Pediatric Liver Transplant
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: Room 206
Background:
Hepatoblastoma (HB), hepatocellular carcinoma (HCC), along with hemangioendothelioma, hemangiosarcoma, and angiosarcoma (HHA) are rare tumors in children that are treated with orthotopic liver transplantation (OLT) when partial hepatectomy is not feasible.
Purpose:
The purpose of this study was to examine the effect of era and patient age on late outcomes after OLT in the management of pediatric malignant tumors.
Methods:
Pediatric (<18 years at listing) liver transplant recipients with HB, HCC and HHA were identified using Scientific Registry for Transplant Recipients data from 1987 to 2014. Graft and patient survival were analyzed using Kaplan-Meier and multivariable Cox proportional hazards regression methods.
Results:
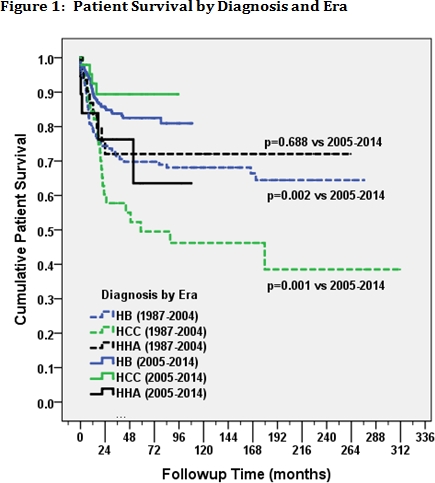
Six hundred forty-one OLTs (489 HB, 97 HCC, 55 HHA; 241 during 1987-2004, 400 during 2005-2014) were performed in 603 patients (5% with >1 OLT). Overall follow-up time averaged 66±75 months (range: <1 to 312) and did not differ between the three tumor types (p=0.371). While there were no differences in overall graft (p=0.096) or patient survival (p=0.170) between the three tumor types, graft and patient survival were better overall (both p≤0.001) in the more recent era for HB and HCC [Figure 1]. After adjusting for previous abdominal surgery (p=0.147), HB recipients in the upper quartile for age at OLT (>45 months) had a 72% increased risk (HR=1.72, 95%CI: 1.03-2.86, p=0.037) of failure of the first/only graft compared to those in the lower quartile (≤18 months).
Conclusions:
Long-term outcomes after OLT for primary pediatric malignant tumors have improved during the last decade for patients having HB or HCC, but not for patients with HHA. Younger patients with HB had better initial graft survival rates after OLT. The low retransplant rate and excellent long-term graft and patient survival rates demonstrate the benefits of OLT when partial hepatectomy is not possible.
CITATION INFORMATION: Patel R, Feurer I, Karp S, Gillis L, Katzenstein H, Lovvorn III H, Pietsch J, Chung D, Tiao G, Hanto D. Long-Term Outcomes After Pediatric Liver Transplantation for Malignant Liver Tumors: Effects of Era and Age. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Patel R, Feurer I, Karp S, Gillis L, Katzenstein H, III HLovvorn, Pietsch J, Chung D, Tiao G, Hanto D. Long-Term Outcomes After Pediatric Liver Transplantation for Malignant Liver Tumors: Effects of Era and Age. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/long-term-outcomes-after-pediatric-liver-transplantation-for-malignant-liver-tumors-effects-of-era-and-age/. Accessed February 18, 2026.« Back to 2016 American Transplant Congress
