Long-Term Insulin Independence Achieved by a Multimodal Approach to Beta-Cell Replacement in Patients with Type I Diabetes
1Surgery, University of California, San Francisco, San Francisco, CA, 2Cedars-Sinai Medical Center, Los Angeles, CA, 3University of California, San Francisco, San Francisco, CA, 4University of California San Francisco, San Francisco, CA, 5UCSF Medical Center, San Francisco, CA, 6Univ of California-San Francisco, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1149
Keywords: Immunosuppression, Islets, Pancreas transplantation, Tolerance
Topic: Clinical Science » Pancreas » 65 - Pancreas and Islet: All Topics
Session Information
Session Name: Pancreas and Islet: All Topics
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Long-term insulin independence in beta-cell replacement, via islet or pancreas transplant, remains limited by the toxic effects of calcineurin inhibitors (CNI) on beta cells and renal function. Here, we report a multimodal approach including islet and pancreas after islet (PAI) transplant utilizing CNI-free immunosuppression (IS) regimens based on Belatacept (BELA) and Efalizumab (EFA).
*Methods: Ten patients with severe Type 1 diabetes (T1D) received their first islet transplant between 2007 and 2009 with CNI-sparing IS based on BELA (n=5) or EFA (n=5). Patients were monitored for a mean of 12.9±1.1 years for beta cell function and renal function. Following islet failure, patients were considered for repeat islet infusion and/or PAI transplant. Circulating immunologic phenotype was characterized in the first year.
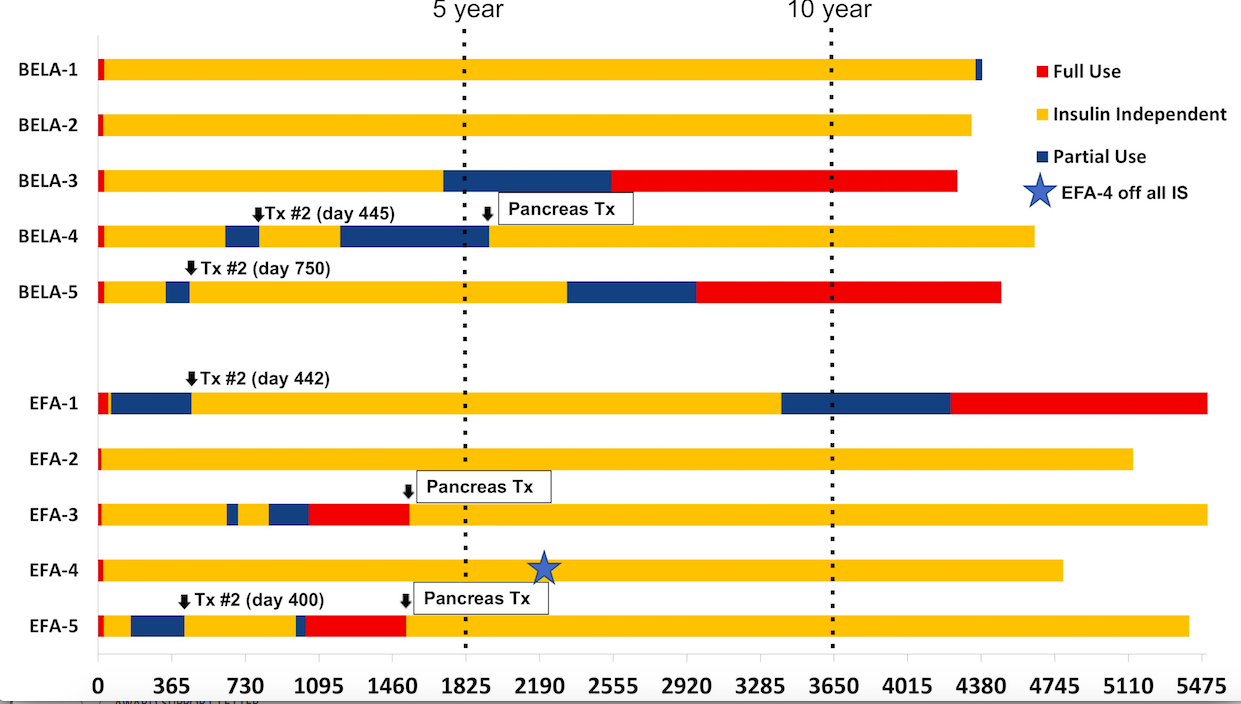
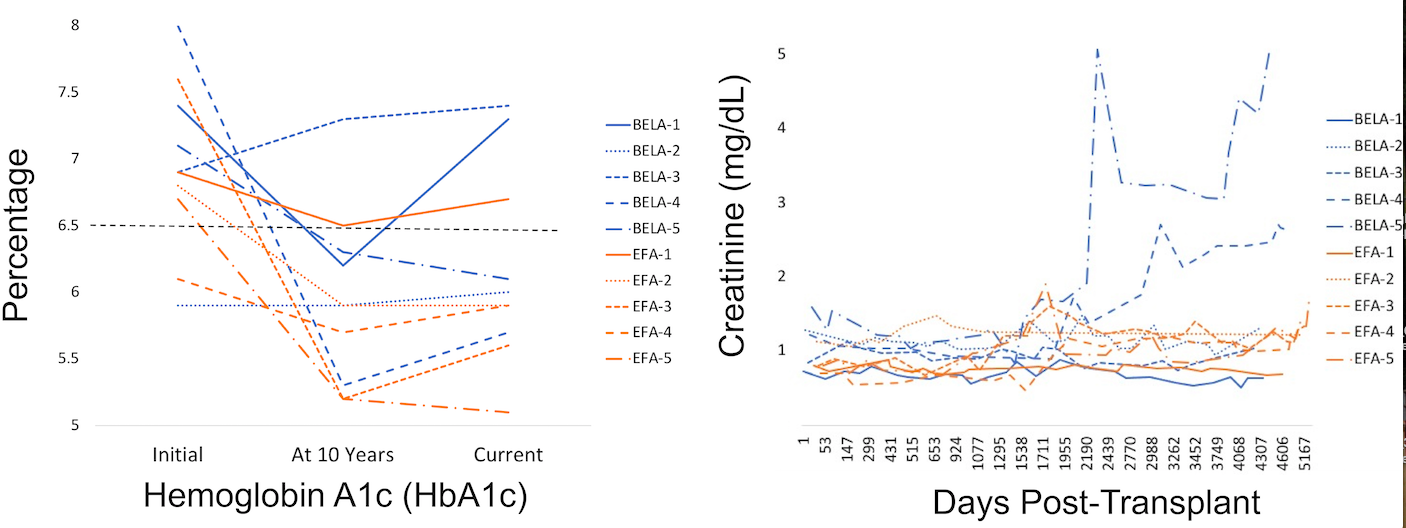
*Results: Seven of 10 patients (70%) maintained insulin independence (3 BELA, 4 EFA) at 10 years from islet transplant; four patients (2 EFA, 2 BELA) after one islet infusion and three patients (2 EFA, 1 BELA) following PAI transplant (Fig 1 and 2). Six of 10 (60%) remain insulin independent at a mean follow-up of 13.3±1.1 years. Eight of 10 patients maintain renal function with less than 30% decrease in GFR (Figure 2B). Patients receiving EFA demonstrated profound expansion of circulating CD4+Foxp3+ regulatory T cells (Tregs). One patient (EFA-4) with peak Tregs comprising 68% of all circulating CD4+ T cells remains insulin independent despite discontinuing all IS, demonstrating operational tolerance.
*Conclusions: Our results describe a multi-modal, personalized approach to beta-cell replacement in T1D. In our series, repeat islet transplant is ineffective at restoring insulin independence. PAI results in durable insulin independence but was associated with impaired renal function in 1/3 of recipients secondary to CNI dependence.
To cite this abstract in AMA style:
Nunez M, Wisel S, Gardner J, Worner G, Roll G, Syed S, Szot G, Tavakol M, Johnson K, Posselt A, Stock P. Long-Term Insulin Independence Achieved by a Multimodal Approach to Beta-Cell Replacement in Patients with Type I Diabetes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/long-term-insulin-independence-achieved-by-a-multimodal-approach-to-beta-cell-replacement-in-patients-with-type-i-diabetes/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress