Liver Allograft Hepatitis and Graft Loss After Hepatitis C Clearance.
D. Bruno, S. Brown, S. Hanish, J. LaMattina, W. Hutson, S. Kottilil, W. Twadell, R. Barth.
Surgery, University of Maryland School of Medicine, Baltimore, MD
Meeting: 2017 American Transplant Congress
Abstract number: D223
Keywords: Graft failure, Hepatitis C, Liver transplantation
Session Information
Session Name: Poster Session D: Liver: Viral Hepatitis
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Successful HCV therapies should improve inferior outcomes of liver transplantation (LT) for HCV cirrhosis. We hypothesize certain patients may be predisposed to heterologous immunity that targets hepatocytes that persist post viral clearance. We report a case series of progressive hepatitis and graft loss with undetectable viral load after LT.
Methods:
IRB-approved retrospective review from 3 liver transplant patients in 2015-6.
Results:
Case 1 – A 39 y/o male was diagnosed with Hepatitis C cirrhosis in 11/2014. He completed treatment and achieved SVR. He underwent LT. He did well but 4 months later was found to have increasing bilirubin. Biopsies showed biliary disease with cholestasis, interface hepatitis, and bile duct proliferation. The hepatitis C viral load remained undetectable. The patient succumbed to liver failure.
Case 2 – A 62 y/o male with hepatitis C cirrhosis and hepatocellular carcinoma was treated pretransplant and achieved SVR. The patient did well after LT and was treated for mild acute rejection. Despite this he continued to have increased bilirubin. Repeated biopsies showed cholestasis with duct damage and spotty confluent necrosis. His viral load was undetectable. The patient succumbed to liver failure.
Case 3 – A 64 y/o male with hepatitis C cirrhosis spontaneously cleared virus prior to receiving an LT. He had an uncomplicated immediate post-operative course. He had increasing LFTs and a biopsy 3 months after transplant was suggestive of recurrent hepatitis C. He had multiple biopsies for increased hepatic enzymes and increased bilirubin that showed portal and periportal (interface) hepatitis with lymphoid aggregate formation. The HCV viral load remained negative. He succumbed to liver failure 6 months after transplant.
Conclusion:
Histologic evidence and clinical course of fibrosing cholestatic hepatitis and graft loss were observed in a series of liver transplant patients cleared of HCV. This series may support the continued presence of deleterious cellular immune responses to hepatocytes after successful HCV therapy.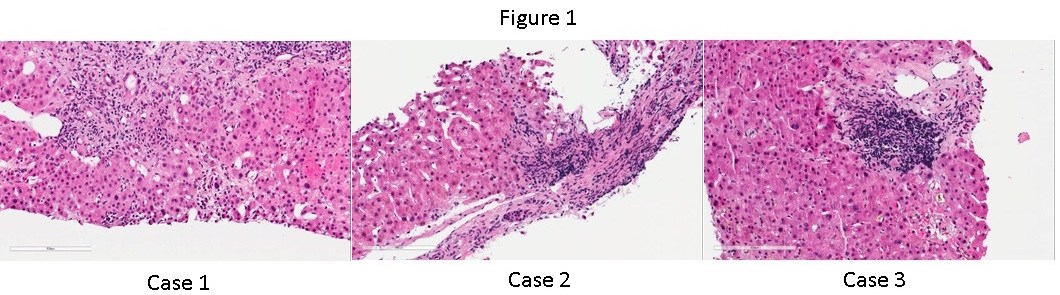
CITATION INFORMATION: Bruno D, Brown S, Hanish S, LaMattina J, Hutson W, Kottilil S, Twadell W, Barth R. Liver Allograft Hepatitis and Graft Loss After Hepatitis C Clearance. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bruno D, Brown S, Hanish S, LaMattina J, Hutson W, Kottilil S, Twadell W, Barth R. Liver Allograft Hepatitis and Graft Loss After Hepatitis C Clearance. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-allograft-hepatitis-and-graft-loss-after-hepatitis-c-clearance/. Accessed February 26, 2026.« Back to 2017 American Transplant Congress
