Kidney Transplants Following Donation after Circulatory Death and Donation after Brain Death Have Similar Early Outcomes
1J.C. Walter, Jr. Transplant Center, Houston Methodist Hospital, Houston, TX, 2Center for Molecular and Translational Human Infectious Diseases Research, Houston Methodist Research Institute, Houston, TX, 3Pharmacy, Houston Methodist Hospital, Houston, TX
Meeting: 2019 American Transplant Congress
Abstract number: B165
Keywords: Donors, non-heart-beating, Graft function, Graft survival, Kidney transplantation
Session Information
Session Name: Poster Session B: Kidney Donor Selection / Management Issues
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Donation after circulatory death (DCD) is common in the US, comprising 18.3% of the deceased donor pool in 2017. Recipient outcomes following DCD kidney transplantation (KT) are incompletely understood.
*Methods: Retrospective review of DCD and DBD KT at a single center performed between 1/2017 and 10/2018. All DCD KT were compared to a matched sample of DBD KT performed during the same time period. Univariate and multiple logistic regression analyses were performed to assess delayed graft function (DGF), acute rejection rate, and renal function (eGFR). Kaplan-Meier curves depicted the risk of graft loss.
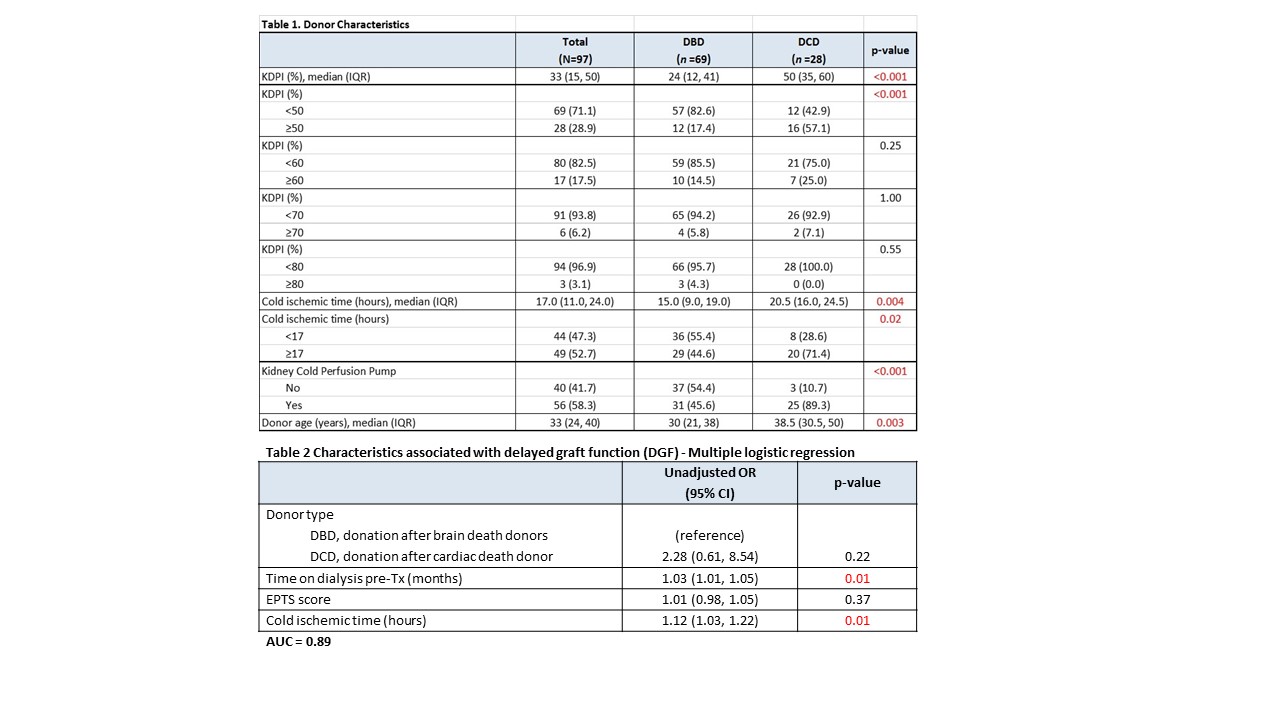
*Results: Recipient characteristics of age, gender, and race were equivalent between groups, however the DCD group had increased median (interquartile range [IQR]) pre-transplant dialysis time (55 [28,84] vs. 33 [12,72] months, p=0.049) and peak % calculated panel reactive antibody (cPRA) (46 [25,95] vs. 30 [2, 68], p=0.03) compared to the DBD group. Donor characteristics were notable for significantly increased donor age, increased kidney donor profile index (KDPI), longer cold-ischemia time (CIT), and increased use of cold perfusion pumping in the DCD versus the DBD group (Table 1). Univariate analysis demonstrated a higher rate of DGF in the DCD vs. group (39.4% vs. 14.5%, p=0.01); however, multiple logistic regression analysis identified increased recipient dialysis time and longer CIT as risk factors for DGF, rather than DCD donor status (Table 2). No differences were detected in the early acute rejection rate (7 vs. 1%, p=0.2), or in median (IQR) eGFR at 3 months (58.5 [45, 70] vs. 62 [46, 74], p=0.26) or at 1-year post-transplant (61 [37, 88] versus 71 [55, 90] ml/min, p=0.39) in the DCD versus DBD groups. The predicted 1-yr graft survivals (Kaplan Meier survival curves) of DCD vs. DBD KT were 94% and 97%, respectively, p=0.83.
*Conclusions: Kidney transplants from DCD and DBD donors had similar outcomes, including 1-year graft survival. The elevated incidence of DGF in the DBD cohort may be attenuated by reducing CIT through more efficient organ placement. Transplant centers should consider DCD donors to be an important source of high-quality organs for kidney transplantation.
To cite this abstract in AMA style:
Hobeika M, Nguyen D, Graviss E, Gaber A, Podder H, Yi S, Kuten S, Patel S, Knight R. Kidney Transplants Following Donation after Circulatory Death and Donation after Brain Death Have Similar Early Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-transplants-following-donation-after-circulatory-death-and-donation-after-brain-death-have-similar-early-outcomes/. Accessed February 28, 2026.« Back to 2019 American Transplant Congress