Kidney Transplantation in Inherited Kidney Diseases
1Division of Nephrology, Saint Louis University, Saint Louis, MO, 2Division of Nephrology, Istanbul Faculty of Medicine, Istanbul, Turkey, 3Department of Pathology, Istanbul Faculty of Medicine, Istanbul, Turkey, 4Center for Abdominal Transplantation, Saint Louis University, Saint Louis, MO, 5Department of Medical Biology, Istanbul Faculty of Medicine, Istanbul, Turkey
Meeting: 2020 American Transplant Congress
Abstract number: D-269
Keywords: Genomics, Graft failure, Kidney transplantation
Session Information
Session Name: Poster Session D: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: We aimed to evaluate the kidney transplant (KTx) recipients with inherited kidney diseases and investigate the causal genetic variants in recipients with undetermined etiology.
*Methods: 109 KTx recipients [63 (58%) male; mean age 36±12; 74 (68%) living related, 9 (8%) living unrelated, 26 (24%) donation after cardiac death (DCD) KTx] with inherited kidney diseases were evaluated. Post-KTx clinical outcomes were assessed. Whole exome sequencing (WES) was performed in 29 of these recipients.
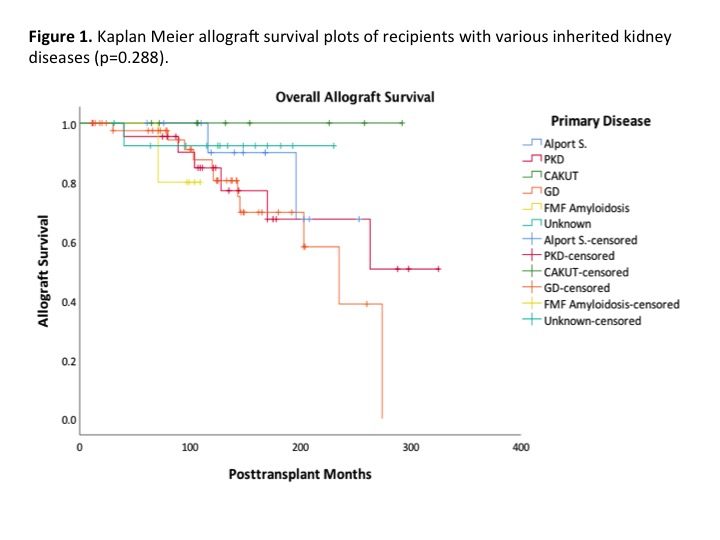
*Results: Primary kidney diseases were as follows: Glomerular diseases (GD) [focal segmental glomerulosclerosis (FSGS) (n=31, 28%), IgA nephropathy (n=7, 6%), MPGN (n=3, 3%), Fabry disease (n=2, 2%), fibrillary glomerulonephritis (n=1 1%) and aHUS (n=1, 1%)]; polycystic kidney disease (PKD) (n=23, 21%); Alport syndrome (n=13, 12%), congenital abnormalities of kidney and urinary tract (CAKUT) (n=9, 8%), AA amyloidosis (n=5, 5%) and unknown (n=14, 13%). CAKUT and GD patients were younger than PKD patients (p<0.001). Defined subgroups did not differ significantly in terms of donor type, HLA mismatch, follow up time, rejection and graft survival (Fig 1).
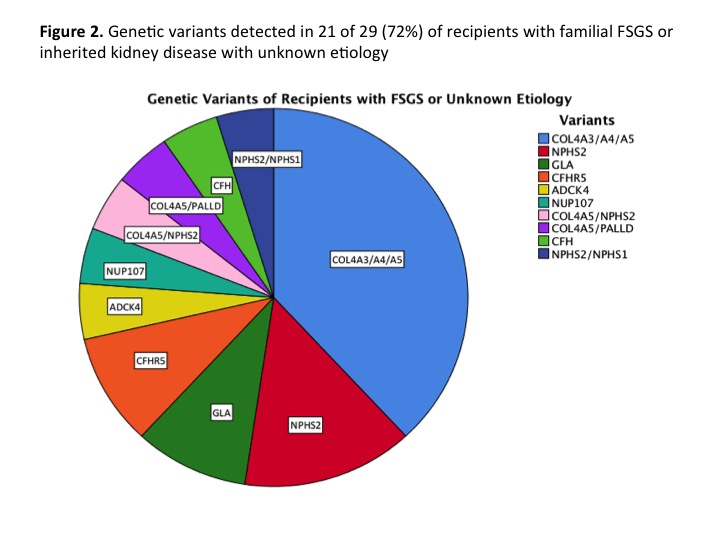
We identified a pathogenic genotype in 21 out of 29 (72%) inherited cases with FSGS or unknown etiology (Fig 2).
Only one of the living related donors (1.35%) of this cohort developed proteinuria and kidney biopsy showed FSGS.
*Conclusions: The outcomes of KTx from a living related, unrelated or DCD donors were similar in recipients with inherited kidney diseases. However, genetic variants were detected in most of the recipients with FSGS or unknown cause of ESKD. Potential living related donors for patients with inherited kidney diseases needed to be evaluated carefully for the presence of genetic variants before a decision is made for kidney donation.
To cite this abstract in AMA style:
Caliskan Y, Yazici H, Ouseph R, Ozluk Y, Randall H, Demir E, Oguz FSavran, Turkmen A, Sever MS, Lentine K. Kidney Transplantation in Inherited Kidney Diseases [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-transplantation-in-inherited-kidney-diseases/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress