Kidney Transplant Outcomes in Patients with ESRD Due to Myeloma
Indiana University School of Medicine, Indianapolis, IN
Meeting: 2019 American Transplant Congress
Abstract number: D341
Keywords: Kidney transplantation, Malignancy, Mortality
Session Information
Session Name: Poster Session D: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Recent literature has suggested that certain patients with multiple myeloma can successfully undergo renal transplantation after stem transplantation with consideration for maintenance therapy. Outcomes of Patients with ESRD due to Myeloma has not been studied extensively. As more and more patients are surviving longer and becoming eligible for transplantation, we examined the outcomes of this population.
*Methods: The UNOS/OPTN database was analyzed for all cases from 1998 to 2017 for ESRD due to Myeloma (Code 3023). Multi-organ transplants were excluded.
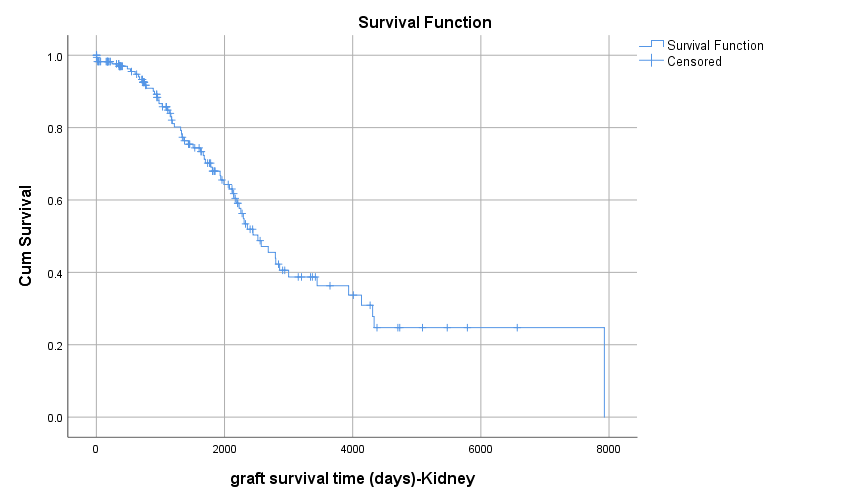
*Results: A total of 176 cases were identified. 1,3,5, 10 year uncensored graft survival was 97,86,68,37 % respectively, whereas death-censored graft survival was 98,95,93,89 % respectively. The patient survival was 99,92, 74 37% at 1,3,5,10 years respectively. There was no difference in graft survival between AA vs Caucasians, Living vs Deceased Donor Transplants or those with or without DGF. (p=0.41). However there was in inferior survival amongst male recipients compared to females (p=0.033).
*Conclusions: We conclude that with careful selection, eligible patients with treated Myeloma have favorable outcomes compared to other non-Myeloma recipients. They tend to have a very low rate of Acute rejections. Further studies are needed to look at other outcomes which may impact survival such as recurrence of myeloma. To our knowledge this is the largest and first study analyzing the outcomes of these patients in the US.
| Variable | Results |
| Mean age at time of Transplant | 53.7+/-10.0 |
| Mean Donor Age | 43.2+/-14.5 |
| Mean BMI | 25.9+/-4.6 |
| Mean Cold Ischemia Time (hrs) | 11.0+/-11.9 |
| Median WaitingTime (days) | 257 (IQR67-676) |
| DM (%) | 2.8 |
| ECD (%) | 4.5 |
| Caucasians/ AA (%) | 82.4/6.3 |
| DGF (%) | 11.4 |
| GenderM/F (%) | 54.5 / 45.5 |
| Zero MM (%) | 16.5 |
| DCD (%) | 5.7 |
| On Dialysistime of Transplant (%) | 68.8 |
| Deceased / Living Donor (%) | 44.8 / 55.1 |
| 1 yr Rejection (%) | 2.8 |
To cite this abstract in AMA style:
Riaz A, Khalil A, Yaqub MS, Taber T, Adebiyi O, Sharfuddin A. Kidney Transplant Outcomes in Patients with ESRD Due to Myeloma [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-transplant-outcomes-in-patients-with-esrd-due-to-myeloma/. Accessed July 18, 2025.« Back to 2019 American Transplant Congress