Induction Immunosuppression Practices in Liver Transplantation are Variable and Predict Post-Transplant Survival
1Gastroenterology, University of Pennsylvania, Philadelphia, PA, 2University of Pennsylvania, Philadelphia, PA
Meeting: 2019 American Transplant Congress
Abstract number: D136
Keywords: Immunosuppression, Induction therapy, Liver transplantation
Session Information
Session Name: Poster Session D: Liver: Immunosuppression and Rejection
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Unlike in other solid organ transplants, the benefits of induction immunosuppression prior to liver transplantation (LT) remain uncertain. The objective of this study was to evaluate center induction practices, recipient predictors of use and its association with post-LT outcomes in a national sample.
*Methods: This was a retrospective cohort study of adult, first-time liver alone recipients (N=54,990) at U.S. centers performing over 50 liver transplants between 2005-2015 using data from the United Network for Organ Sharing.
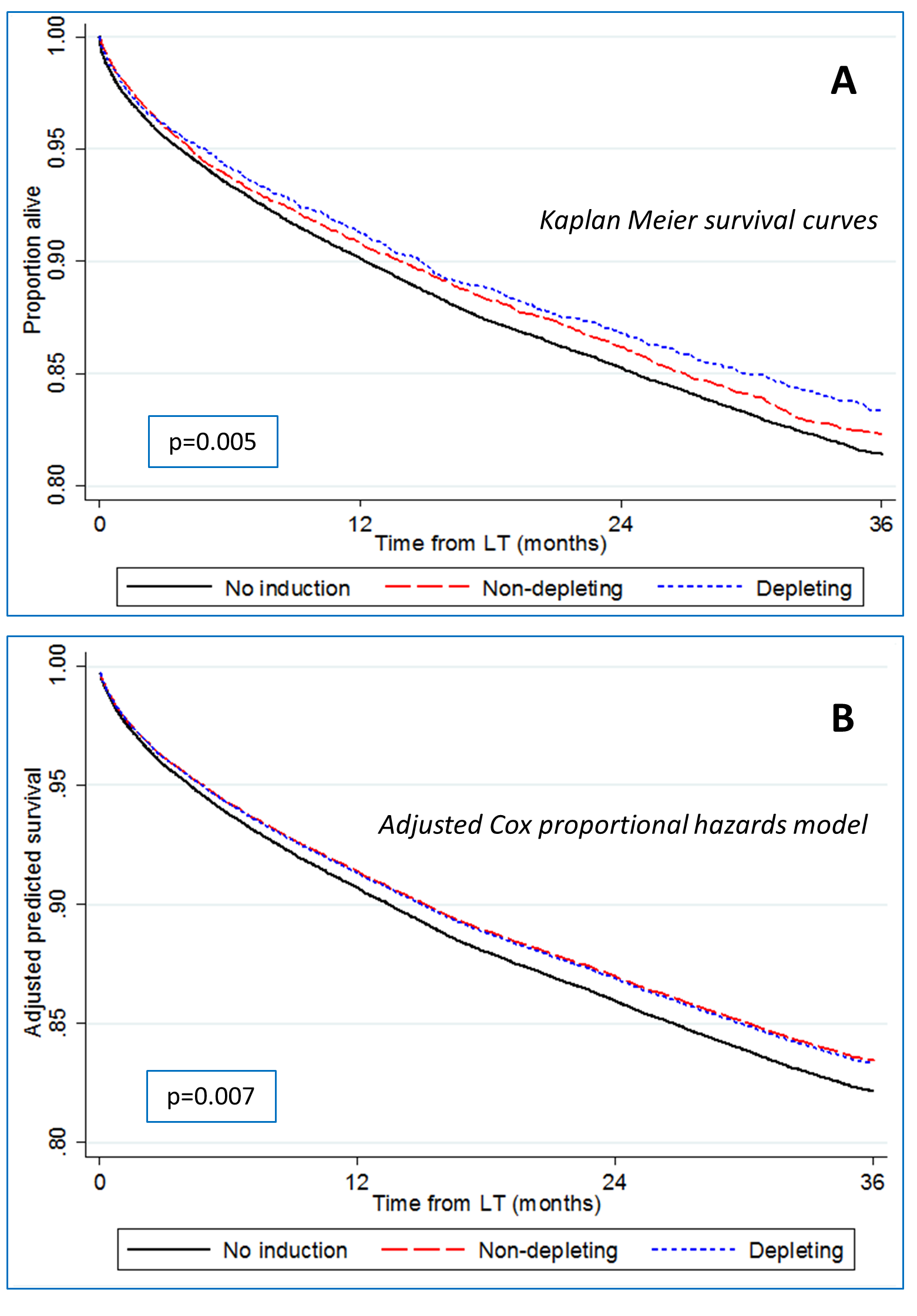
*Results: Overall, 26.2% (N=14,425) of recipients received induction, of which 59.9% received non-depleting and 40.1% received depleting induction. There was significantly more variability in the predicted probability of receiving any induction when accounting for recipient/donor factors and LT center than when accounting for recipient/donor factors alone (variance 0.08 vs 0.007, respectively), indicating that the likelihood of receiving induction was more influenced by center practices. Of 112 centers, 83 (74.1%) used no induction in ≥50% of LTs, while 16 (14.3%) and 6 (5.4%) used non-depleting and depleting induction in a majority of LTs. Receipt of induction was associated with a small but significant reduction in all-cause mortality among recipients in both unadjusted (Figure – Panel A) and adjusted analyses (Figure – Panel B). Accounting for center correlation, recipient/donor factors and temporal trends, the adjusted hazard ratio for mortality was 0.92 (95% CI: 0.87-0.98) with non-depleting induction and 0.93 (95% CI: 0.86-1.00) with depleting induction, using no induction as reference.
*Conclusions: While a majority of patients do not receive induction for LT, clusters of increased utilization exist that are in large part driven by center preference, and overall adjusted post-LT mortality is lower in those receiving induction.
To cite this abstract in AMA style:
Bittermann T, Hubbard R, Lewis J, Goldberg D. Induction Immunosuppression Practices in Liver Transplantation are Variable and Predict Post-Transplant Survival [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/induction-immunosuppression-practices-in-liver-transplantation-are-variable-and-predict-post-transplant-survival/. Accessed March 7, 2026.« Back to 2019 American Transplant Congress