Incidence of Epstein Barr Virus (EBV) DNAemia in EBV-Seronegative Solid Organ Transplant (SOT) Recipients with EBV-Seropositive Donors
1Pediatrics, University of Alberta, Edmonton, Canada
2Medicine, University of Alberta, Edmonton, Canada.
Meeting: 2018 American Transplant Congress
Abstract number: B365
Keywords: Monitoring, Pediatric, Post-transplant lymphoproliferative disorder (PTLD)
Session Information
Session Name: Poster Session B: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Purpose: Since 2002, a pre-emptive approach to post-transplant lymhoproliferative disease prevention has been used at our center that includes EBV viral load (VL) monitoring in whole blood weekly from week 4-20 then monthly from month 6-12 and 3 months of anti-viral prophylaxis with valganciclovir/ganciclovir in EBV-mismatched SOT recipients (donor EBV seropositive(D+)/recipient EBV seronegative (R-)). We investigated the incidence of EBV DNAemia in D+/R- adult and pediatric SOT recipients according to donor and recipient age and organ transplanted.
Methods: To account for passive maternal antibody, seropositive recipients <12 mos of age at transplant were considered R-, while EBV-seropositive donors <12 mos were considered D+. We explored the association between incidence of EBV DNAemia and variables including recipient age group, donor age group and organ group using cumulative incidence curves. Curves were compared using log-rank test. EBV infection within 1 year post-transplant was considered likely donor-acquired and likely community acquired after 1 year.
Results: Between 2002-2016, 256 D+/R- SOT recipients (kidney or kidney+pancreas n=63, heart n=75, liver n=93, lung or heart+lung n=25) were available for analysis. The incidence of post-transplant EBV DNAemia by recipient and donor age and allograft type is illustrated in figure 1. 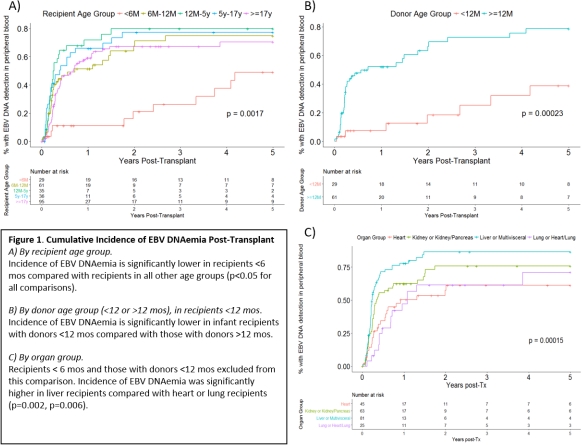 Only 3/29 (10.3%) recipients <6 mos (0.8, 3.6, 4.6 mos) had detectable EBV DNAemia within 1 yr post-transplant; the respective donors were 2.5 mos, 3.8 yrs and 2.9 mos old.
Only 3/29 (10.3%) recipients <6 mos (0.8, 3.6, 4.6 mos) had detectable EBV DNAemia within 1 yr post-transplant; the respective donors were 2.5 mos, 3.8 yrs and 2.9 mos old.
Conclusion: Incidence of donor-acquired EBV infection is high in EBV mismatched recipients >6 mos of age despite anti-viral prophylaxis. The lower incidence of EBV DNAemia in infants whose donors were <12 mos compared to those with donors > 12 mos supports that many of these EBV-seropositive donors <12 mos have passive maternal antibody rather than true EBV infection. Given the low incidence of early EBV DNAemia in D+/R- recipients <6 mos, and in recipients <12 mos whose donors are <12 mos, anti-viral prophylaxis and frequent EBV VL monitoring is likely of little benefit in these groups.
CITATION INFORMATION: Burton C., Mabilangan C., Preiksaitis J. Incidence of Epstein Barr Virus (EBV) DNAemia in EBV-Seronegative Solid Organ Transplant (SOT) Recipients with EBV-Seropositive Donors Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Burton C, Mabilangan C, Preiksaitis J. Incidence of Epstein Barr Virus (EBV) DNAemia in EBV-Seronegative Solid Organ Transplant (SOT) Recipients with EBV-Seropositive Donors [abstract]. https://atcmeetingabstracts.com/abstract/incidence-of-epstein-barr-virus-ebv-dnaemia-in-ebv-seronegative-solid-organ-transplant-sot-recipients-with-ebv-seropositive-donors/. Accessed July 3, 2025.« Back to 2018 American Transplant Congress
