In Vivo and In Vitro PPAR-y Activation Decreases M1-Macrophage Polarization and Improves Liver Ischemia Reperfusion Injury
1Multi Organ Transplant Program, Toronto General Hospital, Toronto, ON, Canada
2Department of Pathology, Toronto General Hospital, Toronto, ON, Canada
3Laboratory of Medicine and Pathobiology, Toronto General Hospital, Toronto, ON, Canada.
Meeting: 2018 American Transplant Congress
Abstract number: A74
Keywords: Apoptosis, FACS analysis, Necrosis, Warm ischemia
Session Information
Session Name: Poster Session A: Innate Immunity; Chemokines, Cytokines, Complement
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background:M1-Macrophage polarization has been studied as a potential target to decrease inflammatory response in sepsis and inflammation-related diseases. Its role in the setting of inflammatory response during liver ischemia reperfusion injury is unknown.
Methods:Mouse peritoneal macrophages(PM) were stimulated with LPS+INF-y to achieve in vitro M1-polarization. PMs received Rosiglitazone(RGZ-PPAR-y agonist) or vehicle(Ctrl) 1hr before and then together with LPS+INF-y and were incubated for 24hrs. For In vivo experiments, the mice underwent partial liver ischemia and received RGZ or vehicle 24hr and 1hr prior to reperfusion. Liver samples were taken prior and following reperfusion and were analyzed for apoptosis and necrosis with TUNEL and H&E staining, respectively. In vitro and in vivo(Liver) M1-polarization was evaluated by intracellular nitric oxide(NO) production and assessed with fluorescence(RFU-Relative fluorescence units) and flow-cytometry(MFI-Mean Fluorescence Intensity), respectively.
Results:In vitro PPAR-y activation resulted in a significant reduction of NO production(M1-polarization) in the RGZ vs Ctrl group at 24hrs after stimulation(67238±6580RFU vs 101310±7552RFU;p<0.01)(A). In vivo PPAR-y activation prior to liver reperfusion significantly reduced M1-Kupffer cell polarization in the RGZ vs Ctrl group at 6hr(1469±340MFI vs 3069±779MFI;p<0.01) and 24hr(762±340MFI vs 1074±198MFI;p=0.04) following reperfusion(B). TUNEL analysis showed significant reduction in the RGZ vs Ctrl group at 6hr after reperfusion(26.40±2.93 vs 50.13±8.29%;p=0.04). H&E staining revealed almost 50% reduction in the degree of necrosis in RGZ vs Ctrl group (26.66±4.78 vs 45.62±4.57%;p=0.03)(C).
Conclusion:PPAR-y activation prior to reperfusion improves the deleterious effect of liver reperfusion injury by decreasing M1-macrophage polarization.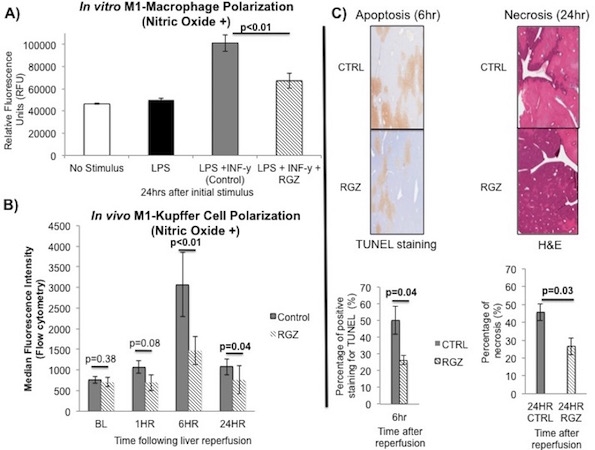
CITATION INFORMATION: Linares I., Bartczak A., Farrokhi K., Kollmann D., Kaths M., Hamar M., Urbanellis P., Ganesh S., Adeyi O., Yip P., Selzner M., Selzner N. In Vivo and In Vitro PPAR-y Activation Decreases M1-Macrophage Polarization and Improves Liver Ischemia Reperfusion Injury Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Linares I, Bartczak A, Farrokhi K, Kollmann D, Kaths M, Hamar M, Urbanellis P, Ganesh S, Adeyi O, Yip P, Selzner M, Selzner N. In Vivo and In Vitro PPAR-y Activation Decreases M1-Macrophage Polarization and Improves Liver Ischemia Reperfusion Injury [abstract]. https://atcmeetingabstracts.com/abstract/in-vivo-and-in-vitro-ppar-y-activation-decreases-m1-macrophage-polarization-and-improves-liver-ischemia-reperfusion-injury/. Accessed March 6, 2026.« Back to 2018 American Transplant Congress
