Impact of Rituximab Induction Therapy on Donor-specific Anti-HLA Antibodies in Abo-compatible Kidney Transplant Recipients
1Department of Urology, Tokyo Women's Medical University, Tokyo, Japan, 2Department of Organ Transplant Medicine, Tokyo Women's Medical University, Tokyo, Japan
Meeting: 2021 American Transplant Congress
Abstract number: 956
Keywords: CD20, HLA antibodies, Kidney transplantation, Living donor
Topic: Clinical Science » Kidney » Kidney Living Donor: Long Term Outcomes
Session Information
Session Name: Kidney Living Donor: Long Term Outcomes
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Development of de novo donor-specific anti-HLA antibodies (dnDSA) after kidney transplantation remains strongly associated with antibody-mediated rejection (AMR), which leads to poor graft outcome. Anti-CD20 antibody, rituximab (RXM) plays a role in inhibiting the B cell allo-response immunity in AMR process. This study evaluated the efficacy of RXM as an induction therapy in kidney transplant patients with or without dnDSA development. We also performed a comparative study on the graft survival rates in transplant recipients with/without rituximab RXM treatment as well as with/without de novo antibody development.
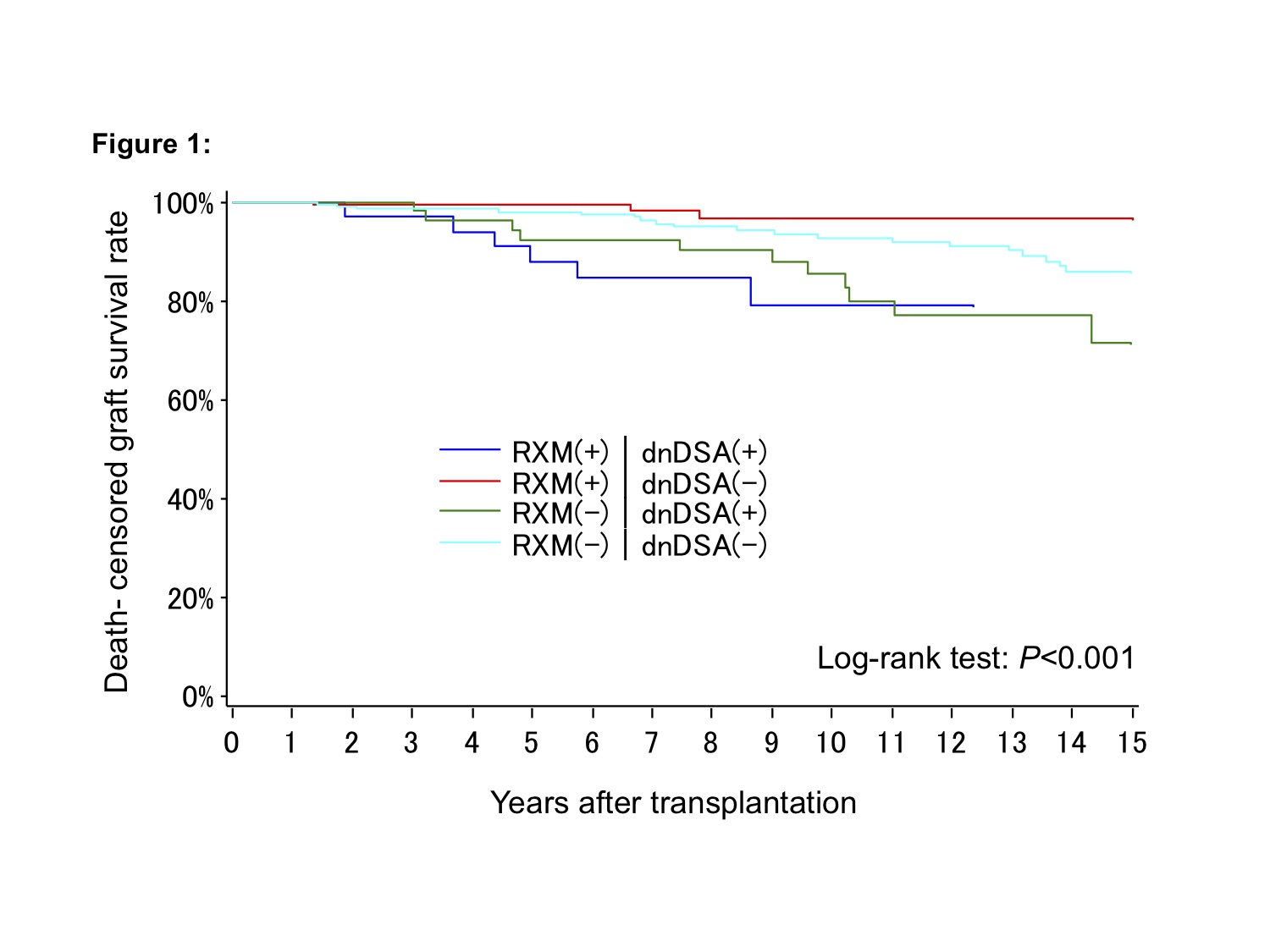
*Methods: We retrospectively analyzed the data of 432 patients who underwent ABO-compatible living kidney transplantation at our institution between 2001 and 2015. Conditions of almost all patients were managed with tacrolimus and mycophenolate mofetil. Preoperative RXM induction was observed in 177 (40.9%) of the 432 patients (RXM+). Low-dose RXM 200mg was administered within 7 days before transplantation. Eighty-five (19.6%) patients (dnDSA+) were positive for dnDSA. Based on RXM induction and dnDSA production, the patients were divided into four groups as follows: RXM(+)/dnDSA(+) (n=33); RXM(+)/dnDSA(-) (n=144); RXM(-)/dnDSA(+) (n=52); and RXM(-)/dnDSA(-) (n=203). The median follow-up period was 10 years (range 7.0-14.3 years).
*Results: The graft survival curve comparing each group is shown in Figure 1. Patients with dnDSA showed poor graft survival than those without dnDSA, regardless of presence/absence of RXM induction. In patients without dnDSA, RXM induction contributed to favorable graft survival. There were significant differences among the four groups (P< 0.001). The most common cause of graft loss in each group was chronic antibody-mediated rejection. The incidence rate of biopsy-proven rejection was significantly higher in the dnDSA(+) groups than that in the dnDSA(-) groups (RXM(+)/dnDSA(+) 60.6%; RXM(+)/dnDSA(-) 11.1%; RXM(-)/dnDSA(+) 55.8%; RXM(-)/dnDSA(-) 25.6%, P<0.001).
*Conclusions: Regardless of RXM induction, the graft survival in dnDSA(-) patients was better than that in dnDSA(+) patients. RXM induction in dnDSA(+) patients was insufficient to achieve the improved graft outcome.
To cite this abstract in AMA style:
Yagisawa T, Kanzawa T, Unagami K, Furusawa M, Inui M, Ishida H, Tanabe K. Impact of Rituximab Induction Therapy on Donor-specific Anti-HLA Antibodies in Abo-compatible Kidney Transplant Recipients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-rituximab-induction-therapy-on-donor-specific-anti-hla-antibodies-in-abo-compatible-kidney-transplant-recipients/. Accessed February 20, 2026.« Back to 2021 American Transplant Congress