Impact of Pretransplant Pregnancy On Immunization and Immunologic Outcome in Kidney Transplantation
1Nephrology, Charité
Universitätsmedizin, Berlin, Germany
2Zentrum für Transfusionsmedizin, Charité
Universitätsmedizin, Berlin, Germany.
Meeting: 2015 American Transplant Congress
Abstract number: 16
Keywords: Alloantibodies, Graft function, HLA antibodies, HLA matching
Session Information
Session Name: Concurrent Session: Deceased Donor Management
Session Type: Concurrent Session
Date: Sunday, May 3, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 2:51pm-3:03pm
Presentation Time: 2:51pm-3:03pm
Location: Room 119-A
BACKGROUND:
The detailed impact of pretransplant pregnancy on HLA alloimmunization and outcome after kidney transplantation is so far not well known.
PATIENTS AND METHODS:
A retrospective single center long-term observational study was conducted. 397 female patients (pts) with end-stage renal disease and no prior transplantation were enrolled in the study. The pts were initially screened before a possible kidney transplantation between 1999 and 2014. 204 of these women received consecutively a kidney transplant. Baseline characteristics including history of transfusion and pregnancy as well as pretransplant and if applicable posttransplant solid phase HLA-diagnostic and immunologic outcome were assessed over a maximum of 15 years.
RESULTS:
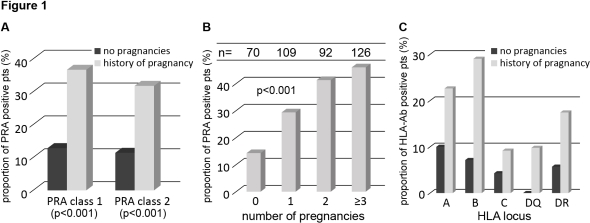
Pts with a history of pregnancy had a significantly higher alloimmunization rate than nulliparous pts (patients with anti-HLA class I 37% vs. 13%, p<0.001 and anti-HLA class II 32% vs. 11%, p<0.001, fig. 1A). The rate of immunized pts increased with the number of pregnancies significantly (fig. 1B). Differentiation of the type of HLA-antibodies depending on the history of pregnancy is shown in figure 1C. The multivariate analysis adjusted for age and history of transfusion identified pregnancy as an independent risk factor for HLA-immunization (OR 3.94, p<0.001). 204 of the women were so far transplanted. After 7 years of follow-up women with a history of pregnancy vs. nulliparous women showed no significant difference regarding the predicted incidence of antibody-mediated rejections (3% vs. 1%, p=0.243), T-cell mediated rejections (19% vs. 24%, p=0.597) and graft failure (8% vs.18%, p=0.556).
CONCLUSION:
Pregnancies constitute a strong risk factor for the development of HLA antibodies in solid organ transplantation. Due to careful selection of donors with avoidance of preformed DSA-antibodies the impact on the immunologic outcome can be minimized.
To cite this abstract in AMA style:
Staeck O, Khadzhynov D, Kreimer S, Rajakangas E, Schönemann C, Lachmann N, Budde K, Halleck F. Impact of Pretransplant Pregnancy On Immunization and Immunologic Outcome in Kidney Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-pretransplant-pregnancy-on-immunization-and-immunologic-outcome-in-kidney-transplantation/. Accessed March 1, 2026.« Back to 2015 American Transplant Congress
