Impact of Positive Crossmatch Due to Non-HLA Antibodies on Graft Outcomes in Renal Transplantation
Houston Methodist Hospital, Houston, TX.
Meeting: 2015 American Transplant Congress
Abstract number: D153
Keywords: Alloantibodies, HLA antibodies, Rejection
Session Information
Session Name: Poster Session D: Kidney: Acute Rejection
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
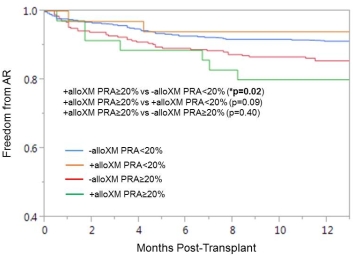
Location: Exhibit Hall E
It is widely recognized that a positive allogeneic crossmatch (+alloXM) due to pre-existing human leukocyte antigen (HLA) antibodies is associated with early rejection episodes. However, the significance of +alloXM due to non-HLA antibodies remains poorly defined. The purpose of this study was to compare graft outcomes at 1 year in renal transplant recipients (RTRs) with +alloXM due to non-HLA antibodies to those with a negative allogeneic crossmatch (-alloXM). RTRs from 5/2007 to 9/2013 were reviewed. Patients that received desensitization, those with +alloXM due to HLA antibodies, and +alloXM patients with positive autologous crossmatch (+autoXM) or missing +autoXM results were excluded. The overall incidence of +alloXM was 68/876 (8%). T-cell crossmatch was positive in 53 cases and B-cell crossmatch in 42; both were positive in 21 patients. Baseline demographics are below; the +alloXM group was younger, predominantly female, with higher rates of retransplant and sensitized recipients. Rates of delayed graft function were similar (4% vs 8%, p=0.3). Allogeneic crossmatch results did not impact acute rejection (AR) at 1 year (13% vs 11%, p=0.6) or median time to AR (3.2 [1.4-6.9] vs 3.3 [1.0-5.2] months, p=0.7). However, significantly higher rates of AR were observed among sensitized +alloXM patients (Fig 1). Additionally, +alloXM patients had higher rates of de novo donor specific antibody (25% vs 18%, p=0.2) and antibody-mediated rejection (6% vs 2%, p=0.05) at 1 year. One-year graft loss was comparable (3% vs 4%, p=0.7). Our data suggests that +alloXM due to pre-existing non-HLA antibodies may influence AR, particularly in sensitized patients, while maintaining similar graft survival at 1 year. The impact of non-HLA antibodies on short- and long-term graft outcomes certainly warrants further investigation.
| +alloXM (n=68) | -alloXM (n=808) | p-value | |
| Age, years | 47±13.8 | 50±13.8 | 0.05 |
| Female, n(%) | 41(60%) | 312(39%) | <0.01 |
| African American, n(%) | 19(28%) | 204(25%) | 0.66 |
| Deceased Donor, n(%) | 35(51%) | 484(60%) | 0.17 |
| Retransplant, n(%) | 8(12%) | 44(5%) | 0.05 |
| Peak PRA ≥20%, n(%) | 36(53%) | 293(36%) | <0.01 |
To cite this abstract in AMA style:
Kuten S, Patel S, Land G, Eagar T, Knight R, Loucks J, Gaber L, Gaber A. Impact of Positive Crossmatch Due to Non-HLA Antibodies on Graft Outcomes in Renal Transplantation [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-positive-crossmatch-due-to-non-hla-antibodies-on-graft-outcomes-in-renal-transplantation/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
