Impact of HLA-DR Matching on HLA-DQ Matching Status and the Development of Anti-HLA-DQ De Novo DSA under Calcineurin Inhibitor or Belatacept Immunosuppression
1Terasaki Research Institute, Los Angeles, CA, 2Emory University, Atlanta, GA, 3Bristol-Myers Squibb, Princeton, NJ
Meeting: 2019 American Transplant Congress
Abstract number: A271
Keywords: HLA antibodies, HLA matching, Kidney transplantation
Session Information
Session Name: Poster Session A: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: De novo donor-specific HLA antibodies (dnDSA) that develop after kidney transplantation target more frequently allo-HLA-DQ antigens in comparison to other allo-HLA antigens. Yet, organ allocation schemes only consider HLA-DR antigens matches/mismatches, but not HLA-DQ antigens matches/mismatches with regard to awarding allocation points. In this study, we evaluatedthe impact of HLA-DR matching/mismatching on HLA-DQB1 matching and on the development of anti-HLA-DQ dnDSA across different immunosuppression treatments.
*Methods: We evaluated 291 kidney transplant recipients from the BENEFIT and BENEFIT-EXT trials who received cyclosporine (n=97) or belatacept (n=194) as first-line immunosuppression and who had been low resolution HLA typed for HLA-A/B/DRB1/DQB1 antigens. HLA antibody screening and DSA characterization was performed centrally by solid-phase flow cytometry (One Lambda).
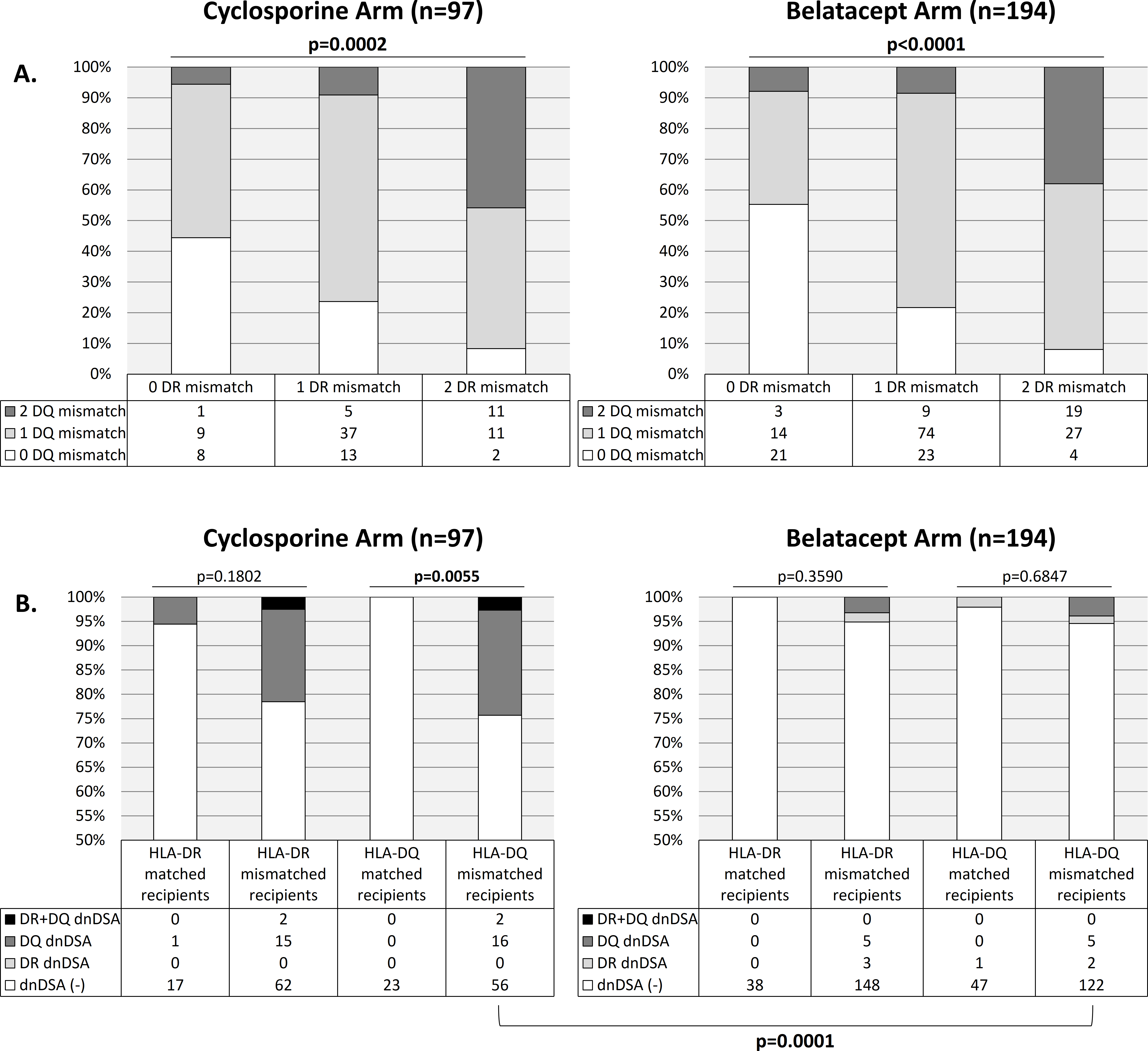
*Results: Among both cyclosporine and belatacept arms, there was a significant association between HLA-DR and -DQ mismatch levels (p=0.0002 and p<0.0001, respectively). Interestingly, 55.6% (cyclosporine arm) and 44.7% (belatacept arm) of HLA-DR matched recipients were mismatched for HLA-DQ. Among both cyclosporine and belatacept arms, respectively, 8.2% and 10.8% of the recipients were matched for HLA-DR and -DQ, 10.3% and 8.8% were matched for HLA-DR only, 15.5% and 13.9% were matched for HLA-DQ only, and 66% and 66.5% were mismatched for both HLA-DR and -DQ (Figure 1A). In the cyclosporine arm, HLA-DR matched recipients (compared to HLA-DR mismatched recipients) did not have a significantly lower development of HLA-DQ dnDSA . In contrast, cyclosporine treated HLA-DQ matched recipients had a significantly lower development of HLA-DQ dnDSA compared to HLA-DQ mismatched recipients (p=0.0055) and did not develop HLA-DR dnDSA. Importantly, belatacept (compared to cyclosporine) was associated with a significantly reduced development of HLA-DQ dnDSA in HLA-DQ mismatched recipients (p=0.0001) (Figure 1B).
*Conclusions: This research indicates that HLA-DR matching leaves a large proportion of recipients still mismatched for HLA-DQ. As a result, matching for HLA-DR did not significantly result in avoidance of HLA-DQ dnDSA development. To prevent HLA-DQ dnDSA, it may be better to HLA-DQ match recipients or potentially use a belatacept based immunosuppression regimen in HLA-DQ mismatched recipients.
To cite this abstract in AMA style:
Jucaud V, Gebel H, Bray R, Polinsky M, Everly M. Impact of HLA-DR Matching on HLA-DQ Matching Status and the Development of Anti-HLA-DQ De Novo DSA under Calcineurin Inhibitor or Belatacept Immunosuppression [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-hla-dr-matching-on-hla-dq-matching-status-and-the-development-of-anti-hla-dq-de-novo-dsa-under-calcineurin-inhibitor-or-belatacept-immunosuppression/. Accessed July 5, 2025.« Back to 2019 American Transplant Congress