Impact of Graft Type, Presence and Type of Inflammatory Bowel Disease on Outcomes Following Liver Transplantation for Primary Sclerosing Cholangitis
S. Kumar1, S. Lin2, J. D. Schold3
1Digestive Disease Institute, Cleveland Clinic Abu Dhabi, Abu Dhabi, United Arab Emirates, 2Department of Quantitative Health Sciences, Cleveland Clinic Foundation, Cleveland, OH, 3Center for Populations Health Research, Cleveland Clinic Foundation, Cleveland, OH
Meeting: 2022 American Transplant Congress
Abstract number: 890
Keywords: Donors, non-heart-beating, Liver transplantation, Living donor, Primary sclerosing cholangitis
Topic: Clinical Science » Liver » 59 - Liver: Expanding the Donor Pool* (Liver: MELD Allocation / Donor Issues)
Session Information
Session Name: Liver: Expanding the Donor Pool* (Liver: MELD Allocation / Donor Issues)
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: In Primary sclerosing cholangitis (PSC), concerns exist regarding outcomes following donation after circulatory death (DCD) liver transplantation (LT) due to risk of ischemic cholangiopathy and living donor LT (LDLT) given it’s immune-mediated basis. Also, limited data is available regarding impact of Inflammatory bowel disease (IBD) on outcomes following LT for PSC. Our goal was to evaluate impact of graft type, presence and type of IBD on outcomes following LT for PSC.
*Methods: Using SRTR, retrospective study cohorts of recipients with PSC undergoing solitary LT were constructed over the time period 2010-2020, stratified by graft type – donation after brain death (DBD), DCD, LDLT – as well as presence and type of IBD. Primary outcome measures were graft (GS) and patient survival (PS). A chi-square test was used for categorical and Student’s t-test for continuous variables. Survival comparison was performed using the Kaplan-Meier method with log-rank test and multivariable analysis of outcomes using Cox proportional hazard models.
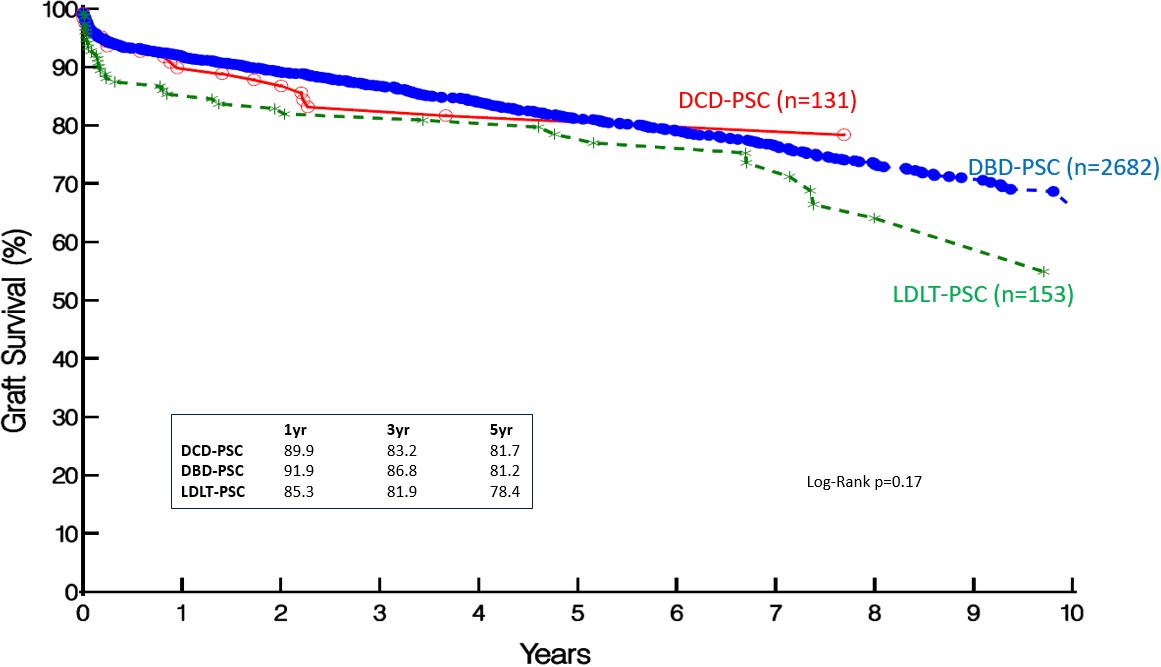
*Results: 2966 recipients underwent LT for PSC over the study period: LDLT-PSC: 53 (5.2%), DCD-PSC: 131 (4.4%) and DBD-PSC: 2682 (90.4%). 1897 had associated IBD (PSC-IBD; 64%): Ulcerative Colitis (UC) in 1483 (78.2%) and Crohn’s disease in 414 (CD; 21.8%). LDLT-PSC recipients were younger (43.9 vs. 48.6 vs. 47.8; p=0.005), with lower BMI, cold ischemia time and MELD score at LT (15.6 vs. 19.6 vs. 23.6; p <.0001). PSC-IBD were younger (46.8 vs. 49.2; p <.0001) than those without IBD. Despite lower MELD at LT, observed GS in LDLT-PSC was lower at 1, 3 and 5 years. However, this did not reach statistical significance (Fig 1). PS was also comparable in all 3 groups. GS and PS in PSC-IBD vs. PSC-non-IBD (p=0.91 and p=0.41 respectively) and PSC-UC vs. PSC-CD were also comparable (p=0.87 and p=0.55 respectively). On multivariable analysis, while donor age was associated with inferior GS (HR (95% CI): 1.01 (1.00 -1.01), p<0.0001), recipient age and cold ischemia time (HR (95% CI): 1.31 (1.04-1.66), p=0.02) were predictive of PS following LT for PSC.
*Conclusions: Outcomes following DCD and LDLT in PSC are comparable to LT using DBD grafts. Presence or type of IBD did not impact outcomes following LT in PSC. Consideration of DCD and LDLT may enable safe expansion of the available donor pool in recipients with PSC, with or without co-existing IBD.
To cite this abstract in AMA style:
Kumar S, Lin S, Schold JD. Impact of Graft Type, Presence and Type of Inflammatory Bowel Disease on Outcomes Following Liver Transplantation for Primary Sclerosing Cholangitis [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-graft-type-presence-and-type-of-inflammatory-bowel-disease-on-outcomes-following-liver-transplantation-for-primary-sclerosing-cholangitis/. Accessed February 20, 2026.« Back to 2022 American Transplant Congress