Impact of Donor Specific Antibodies in the Older Kidney Transplant Recipient
Houston Methodist Hospital, Houston.
Meeting: 2015 American Transplant Congress
Abstract number: 94
Keywords: Age factors, Elderly patients, HLA antibodies, Rejection
Session Information
Session Name: Concurrent Session: Kidney Antibody Mediated Rejection II
Session Type: Concurrent Session
Date: Sunday, May 3, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:48pm-5:00pm
Presentation Time: 4:48pm-5:00pm
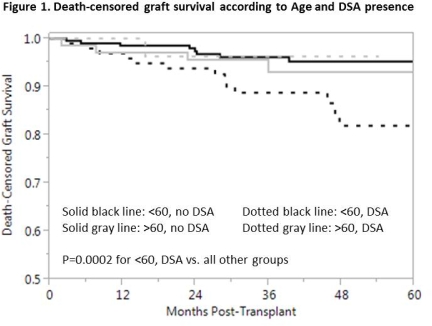
Location: Terrace I-III
Recent evidence suggests that renal transplant recipients (RTR) with both rejection and donor specific antibodies (DSA) are at high risk of graft loss. Concurrently, the average age of RTR is rising. Aging is thought to be associated with a decline in immune function; therefore, the purpose of this study was to describe the incidence and outcomes of de novo DSA in RTR according to age. After excluding patients with pre-transplant DSA, we grouped immunologically high-risk RTR (PRA>20%, retransplants, and African American), by age of > or <60 years. All RTR received antithymocyte globulin, tacrolimus, mycophenolate, and corticosteroids. DSA were checked at 1,3,6, and 12 months or during graft dysfunction. Mean follow-up was 37±19 months. Of 466 RTR reviewed, DSA were detected in 140(30%) at a median of 8 (IQR 3-18) months post-transplant. DSA occurred in a similar proportion of RTR >60 (29/109, 27%) and <60 (111/357, 31%), and occurred earlier post-transplant in the >60 group. As shown below, RTR >60 years had similar percentages of DSA directed against >1 HLA specificity and were as likely to have persistent DSA (>1 occurrence) compared to RTR <60. However, the proportion of "strong" DSA (MFI>8000) was significantly lower among RTR >60. Furthermore, the rates of acute rejection, antibody-mediated rejection and of both rejection and DSA were significantly lower among RTR >60. In contrast to younger RTR, death-censored graft survival in RTR >60 years was not impacted by DSA presence (Figure 1). In conclusion, our data suggests that DSA occur at a similar rate in RTR >60 years, however, they tend to be of weaker intensity and are not associated with deleterious outcomes. These findings indicate that the follow up and management of de novo DSA may be different in high risk patients based on age.
| >60 (n=109) | <60 (n=357) | P-value | |
| DSA occurrence, % | 27 | 31 | 0.36 |
| DSA Characteristics | |||
| Median time to DSA, mos (IQR) | 6 (3-12) | 9 (3-18) | 0.06 |
| >1 DSA specificity, % | 32 | 43 | 0.30 |
| Persistent DSA, % | 50 | 61 | 0.35 |
| DSA MFI>8000, % | 4 | 30 | <0.01 |
| Acute Rejection, % | 12.8 | 21 | 0.05 |
| Antibody-Mediated Rejection, % | 0.9 | 5.3 | 0.02 |
| Acute Rejection AND DSA, % | 4.6 | 12.9 | <0.01 |
To cite this abstract in AMA style:
Patel S, Loucks-DeVos J, Knight R, Kuten S, Gaber L, Gaber A. Impact of Donor Specific Antibodies in the Older Kidney Transplant Recipient [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-donor-specific-antibodies-in-the-older-kidney-transplant-recipient/. Accessed March 7, 2026.« Back to 2015 American Transplant Congress
