Impact of County Health Rankings on Nationwide Liver Transplant Outcomes
S. K. Niazi1, E. Vargas2, A. Spaulding3, J. Crook4, A. P. Keaveny5, T. Schneekloth6, T. Rummans7, C. Taner5
1Psychiatry & Psychology
Transplantation, Mayo Clinic, Jacksonville, FL, 2Heath Services Research, Mayo Clinic, Jacksonville, FL, 3Health Services Research, Mayo Clinic, Jacksonville, FL, 4Health Sciences Research, Mayo Clinic, Jacksonville, FL, 5Transplantation, Mayo Clinic, Jacksonville, FL, 6Psychiatry & Psychology, Mayo Clinic, Rochester, MN, 7Psychiatry & Psychology, Mayo Clinic, Jacksonville, FL
Meeting: 2020 American Transplant Congress
Abstract number: C-262
Keywords: Liver, Liver transplantation, Psychosocial, Survival
Session Information
Session Name: Poster Session C: Non-Organ Specific: Public Policy & Allocation
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: We examined the impact of social determinants of health (SDOH) in LT recipients’ counties of residence and their associations with long-term patient and graft survival.
*Methods: We used United Network for Organ Sharing data to identify adult LT recipients transplanted between January 2010 and June 2018 and used recipient zip codes to link to County Health Rankings (CHR) data. The data include: Heath Outcomes and Health Factors ranks, and Length of Life, Quality of Life, Health Behaviors, Clinical Care, Social and Economic, and Physical Environment sub-ranks. CHR scores were calculated for 3149 US counties for 8 consecutive years. Average CHR scores per county over 8 years were used to create a nationwide rank order list and divided into best, middle & worst tertiles. Mixed effects Cox proportional hazards models were used to examine associations with graft and patient survival post-LT while adjusting for patient, donor, transplant characteristics and random effects of county & transplant center.
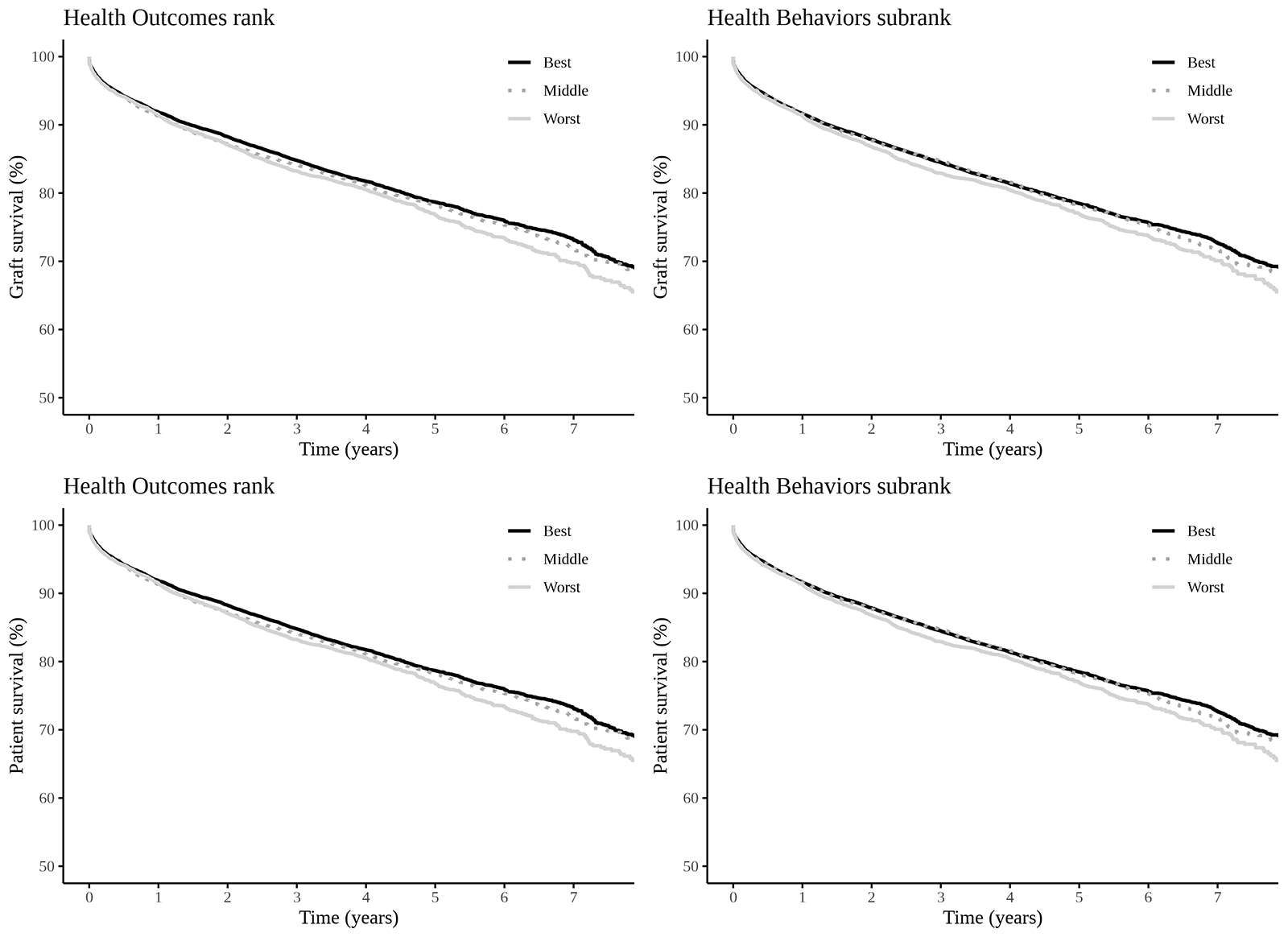
*Results: Among 46,120 LT recipients, Health Outcomes rank was associated with graft failure, with the worst tertile showing 9% increased risk of graft failure compared to the best tertile (95% CI: 1% – 17%, p=0.029). In models including only follow-up outcomes after one-year post-LT, the association with Health Outcomes rank strengthened and Health Behaviors sub-rank was also associated with graft survival, with the worst tertile showing 11% increased risk of graft failure compared to the best tertile (95% CI: 1% – 21%, p=0.040). Health Outcomes rank was also associated with patient survival, with 9% increased risk in worst compared to best tertile counties (95% CI: 1% – 18%, p=0.046). In models including only outcomes after one-year post-transplant, the association with Health Outcomes rank strengthened and Health Behaviors sub-rank was also associated, with patients in the worst tertile counties at an estimated 12% increased risk compared to those in best tertile counties (95% CI: 1% – 22%, p=0.041).
*Conclusions: Recipient’s SDOH in county of residence appear to have statistically significant but modest impacts on outcomes. These factors need to be addressed during the pre-LT assessment to ensure best possible outcomes.
To cite this abstract in AMA style:
Niazi SK, Vargas E, Spaulding A, Crook J, Keaveny AP, Schneekloth T, Rummans T, Taner C. Impact of County Health Rankings on Nationwide Liver Transplant Outcomes [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-county-health-rankings-on-nationwide-liver-transplant-outcomes/. Accessed February 23, 2026.« Back to 2020 American Transplant Congress