Immunologic Impact of Tocilizumab Treatment in Kidney Transplant Recipients with Allograft Inflammation
UCSF, San Francisco.
Meeting: 2018 American Transplant Congress
Abstract number: A136
Keywords: Interferon (IFN), Kidney transplantation, Rejection, T helper cells
Session Information
Session Name: Poster Session A: Kidney Acute Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Proinflammatory cytokine IL-6 increases effector/memory T-cells, induces Th17 cells and prevents the induction of Tregs. IL-6 expression in kidney biopsies is elevated during acute rejection and is correlated with the degree of inflammation. We studied the immunological impact of tocilizumab (TCZ), a monoclonal antibody to the IL-6R in kidney transplant recipients with subclinical graft inflammation
Methods: PBMCs were collected at baseline, 3 and 6 months from stable kidney transplant recipients with subclinical inflammation who had been enrolled in a prospective randomized controlled clinical trial of TCZ (8 mg/kg IV q4 weeks X6 doses) or no treatment (controls) for 6 months. All patients had been maintained on tacrolimus+MMF±prednisone. PBMCs were analyzed with respect to the Treg population, T cell activation, and cytokine (IFN-γ and IL-17) production after ex vivo PMA/Ionomycin stimulation for 4 hours.
Results:
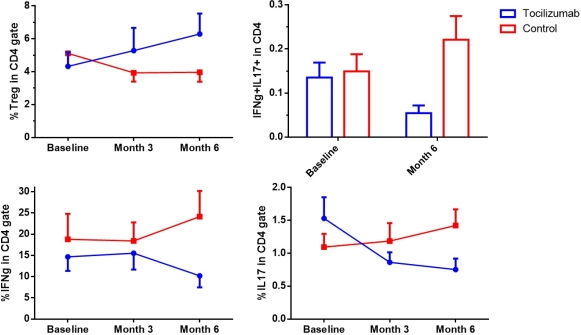
Samples from 20 patients (9 in the TCZ arm and 11 in the control arm) were analyzed. Mean frequency of CD4+CD25+Foxp3+ Tregs was similar in the 2 groups at enrollment (4.3% ± 0.85 vs 5.1% ± 0.76, p= 0.58). At 6 months, the Treg frequency had increased (+50%) in the TCZ group and decreased (-22.5%) in the control group and this difference was significant (p=0.012). The frequencies of naïve (CCR7+CD45RO-), central memory (CCR7+CD45RO+), effector memory (CCR7-CD45RO+), TEMRA (CCR7-CD45RO-) in both CD4 and CD8 T cells remained stable throughout the treatment in both groups.
Patients in the TCZ group showed a profound decline in IFN-γ (-31%) and IL-17 (-51%) production by CD4+ T cells when compared to control group at 6 months. IFN-γ/ IL17 double producing CD4+ T cells also showed a significant decrease in the TCZ group (-60% vs. +48%, p=0.02) at 6 months.
Conclusion:
Tocilizumab treatment for 6 months significantly increased the frequency of peripheral Tregs and suppressed the production of inflammatory cytokines (IFN-γ and IL-17) by circulating effector T cells in kidney transplant recipients with allograft inflammation. The favorable change in Treg to Th17 and Th1 balance suggests that tocilizumab is a promising option for controlling allograft inflammation.
CITATION INFORMATION: Leung J., Chandran S., Vincenti F., Tang Q. Immunologic Impact of Tocilizumab Treatment in Kidney Transplant Recipients with Allograft Inflammation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Leung J, Chandran S, Vincenti F, Tang Q. Immunologic Impact of Tocilizumab Treatment in Kidney Transplant Recipients with Allograft Inflammation [abstract]. https://atcmeetingabstracts.com/abstract/immunologic-impact-of-tocilizumab-treatment-in-kidney-transplant-recipients-with-allograft-inflammation/. Accessed February 28, 2026.« Back to 2018 American Transplant Congress