Identifying the Specific Causes and the Determinants of Outcome in Kidney Recipients with Transplant Glomerulopathy: A Multicenter Study.
1Paris Translational Research Center for Organ Transplantation, Paris, France
2University of Edmonton, Edmonton, Canada
Meeting: 2017 American Transplant Congress
Abstract number: 518
Keywords: Biopsy, Graft failure, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney General Outcomes
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:54pm-5:06pm
Presentation Time: 4:54pm-5:06pm
Location: E354a
Background
Understanding the specific causes of TG and its long-term consequences at population scale is lacking.
Methods
This study includes all kidney allograft biopsies performed between 2004 and 2014 in three French centers and one Canadian center showing TG (Banff cg score≥1 by light microscopy). All TG cases were extensively phenotyped and systematically assessed using light microscopy, immunohistochemistry, immunofluorescence, together with circulating anti-HLA-DSA assessment at the time of biopsy.
Results
Among the 8207 post-transplant biopsies performed during the inclusion period, 559 (6.8%) had double contours and corresponded to 392 patients. Three overlapping etiologies accounted for 467 (84%) cases. 417 biopsies showed alloantibodies-mediated injury (75%), 91 biopsies showed TMA (16%), 65 showed MPGN (12%), while 92 cases (17%) remained equivocal with no specific lesions identified by the pathologist (figure1). The median time to first cg lesion occurrence after transplantation was 32.7 months (IQR: 12.0–77.9). Allograft survival after TG diagnosis was 59% and 41% at 5 and 8 years (figure2). After adjusting for donor, recipient and transplant characteristics, immunological and histological parameters, we identified the following independent factors associated with long-term allograft survival in patients with TG:eGFR (HR:0.96; IC95%(0.95-0.98); p<0.001) and proteinuria level (HR:2.17; IC95%(1.78-2.66); p<0.001) at the time of biopsy, deceased donor (HR:1.64; IC95%(1.11-2.42); p=0.014), delay between transplantation and TG diagnosis (HR:1.34; IC95%(1.18-1.51); p<0.001) and endarteritis Banff scores (HR:1.82; IC95%(1.15-2.88); p=0.002).
Conclusion
Using a large cohort of kidney recipients with a diagnosis of TG and a systematic phenotyping, we identify three overlapping pathways in TG: ABMR, TMA and MPGN. The identification of the main independent determinants of TG prognosis may help improving risk stratification and define specific causes and disease process in patients with TG.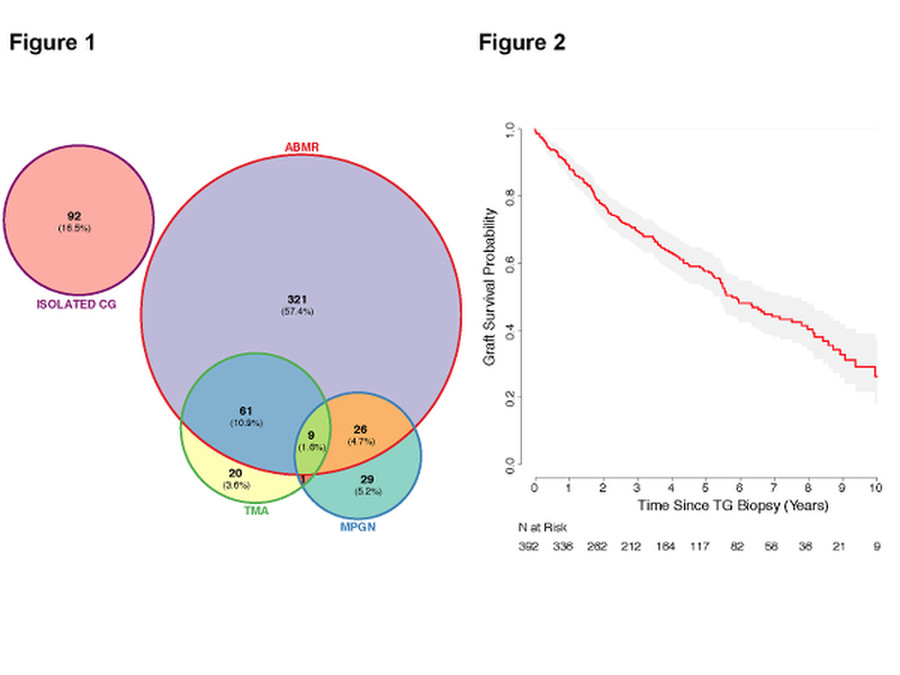
CITATION INFORMATION: Aubert O, Higgins S, Campbell P, Loheac C, Viglietti D, Glotz D, Legendre C, Lefaucheur C, Sis B, Duong Van Huyen J, Loupy A. Identifying the Specific Causes and the Determinants of Outcome in Kidney Recipients with Transplant Glomerulopathy: A Multicenter Study. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Aubert O, Higgins S, Campbell P, Loheac C, Viglietti D, Glotz D, Legendre C, Lefaucheur C, Sis B, Huyen JDuongVan, Loupy A. Identifying the Specific Causes and the Determinants of Outcome in Kidney Recipients with Transplant Glomerulopathy: A Multicenter Study. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/identifying-the-specific-causes-and-the-determinants-of-outcome-in-kidney-recipients-with-transplant-glomerulopathy-a-multicenter-study/. Accessed February 18, 2026.« Back to 2017 American Transplant Congress
