Ideal Outcome After Liver Transplantation: An Exploratory Study Using Machine Learning Analyses to Leverage Long-Term Registry Data from Studies in Pediatric Liver Transplantation (SPLIT).
1University of Washington School of Medicine, Seattle, WA
2Children's Core for Biomedical Statistics, Center for Clinical and Translational Research, Seattle Children's Hospital, Seattle, WA
3The EMMES Corporation, Rockville, MD
4The Hospital for Sick Children and University of Toronto, Toronto, ON, Canada
5Cincinnati Children's Hospital and Medical Center, Cincinnati, OH.
Meeting: 2016 American Transplant Congress
Abstract number: D194
Keywords: Liver transplantation, Outcome, Pediatric
Session Information
Session Name: Poster Session D: Pediatric Liver Transplantation
Session Type: Poster Session
Date: Tuesday, June 14, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
We analyzed the Studies in Pediatric Liver Transplantation (SPLIT) registry dataset using heat map and random forests analyses (RFA) to determine if ideal outcome (IO) at 3 years after liver transplantation (LT) could be predicted from Yr 1 demographic, biochemical and clinical patterns.
Methods: We defined IO as alive at 3y after LT with normal liver tests and eGFR>90 ml/min/m2, alongside absence of disease recurrence, PTLD, and cytopenia. Inclusion criteria: Pts s/p first LT between 2002-2006 for whom the IO parameters at 3y could be determined. A heat map was used to (1) identify distinct pt phenotypes and (2) determine if phenotypes discriminated pts with and without IO. RFA ranked the impact of variables on 3y outcomes.
Results: Amongst 877 SPLIT participants, 334 (38%) had IO. Stepwise addition of demographic, biochemical and clinical variables, including 1[ordm] diagnosis, cold ischemia time, organ type, and primary insurance, did not change the heat map signal. RFA identified non-white race, increased length of operation, rejection, vascular and biliary complications within 30 days, and duct to duct biliary anastomosis to be negatively associated with IO 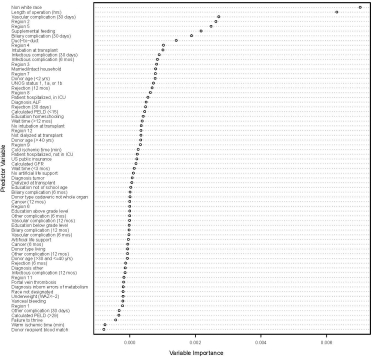 . Varying impact was given to UNOS regions, particularly 2 and 5, which were negatively associated with IO. RFA predicted IO with an accuracy rate of 73.8% (95% CI =70.8% to 76.7%); PPV= 81.8%, NPV = 72.1%.
. Varying impact was given to UNOS regions, particularly 2 and 5, which were negatively associated with IO. RFA predicted IO with an accuracy rate of 73.8% (95% CI =70.8% to 76.7%); PPV= 81.8%, NPV = 72.1%.
Conclusions: Machine learning analyses of SPLIT registry data permitted identification of discrete 1 yr pt phenotypes with varying likelihood of achieving a composite IO at 3y after LT. These findings will inform future studies targeting at-risk LT recipients, and strategies optimizing use of healthcare resources.
CITATION INFORMATION: Hsu E, Shaffer M, Anand R, Ng V, Bucuvalas J. Ideal Outcome After Liver Transplantation: An Exploratory Study Using Machine Learning Analyses to Leverage Long-Term Registry Data from Studies in Pediatric Liver Transplantation (SPLIT). Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Hsu E, Shaffer M, Anand R, Ng V, Bucuvalas J. Ideal Outcome After Liver Transplantation: An Exploratory Study Using Machine Learning Analyses to Leverage Long-Term Registry Data from Studies in Pediatric Liver Transplantation (SPLIT). [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/ideal-outcome-after-liver-transplantation-an-exploratory-study-using-machine-learning-analyses-to-leverage-long-term-registry-data-from-studies-in-pediatric-liver-transplantation-split/. Accessed July 18, 2025.« Back to 2016 American Transplant Congress
