Hypothermic Machine Perfusion Can Improve Hypoxia Tolerance in Human Discarded Liver
The Dumont-UCLA Transplant Center, UCLA, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: 524
Keywords: Ischemia, Liver preservation, Machine preservation
Session Information
Session Name: Basic: Ischemia Reperfusion & Organ Rehabilitation III
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:15pm-4:27pm
Presentation Time: 4:15pm-4:27pm
Location: Virtual
*Purpose: The wider use of livers from expanded criteria donors may help improve access to liver transplantation (LT). Normothermic machine perfusion in LT has been shown to positively increase marginal graft utilization (Nature 2018). Hypothermic machine perfusion (HMP) is cost effective, simple and widely used during kidney transplantation. We sought to employ HMP to better analyze the molecular mechanisms affecting graft function with focus on expression of Hypoxia-inducible factor 1-alpha (Hif1a), a key mediator of cellular response to hypoxia.
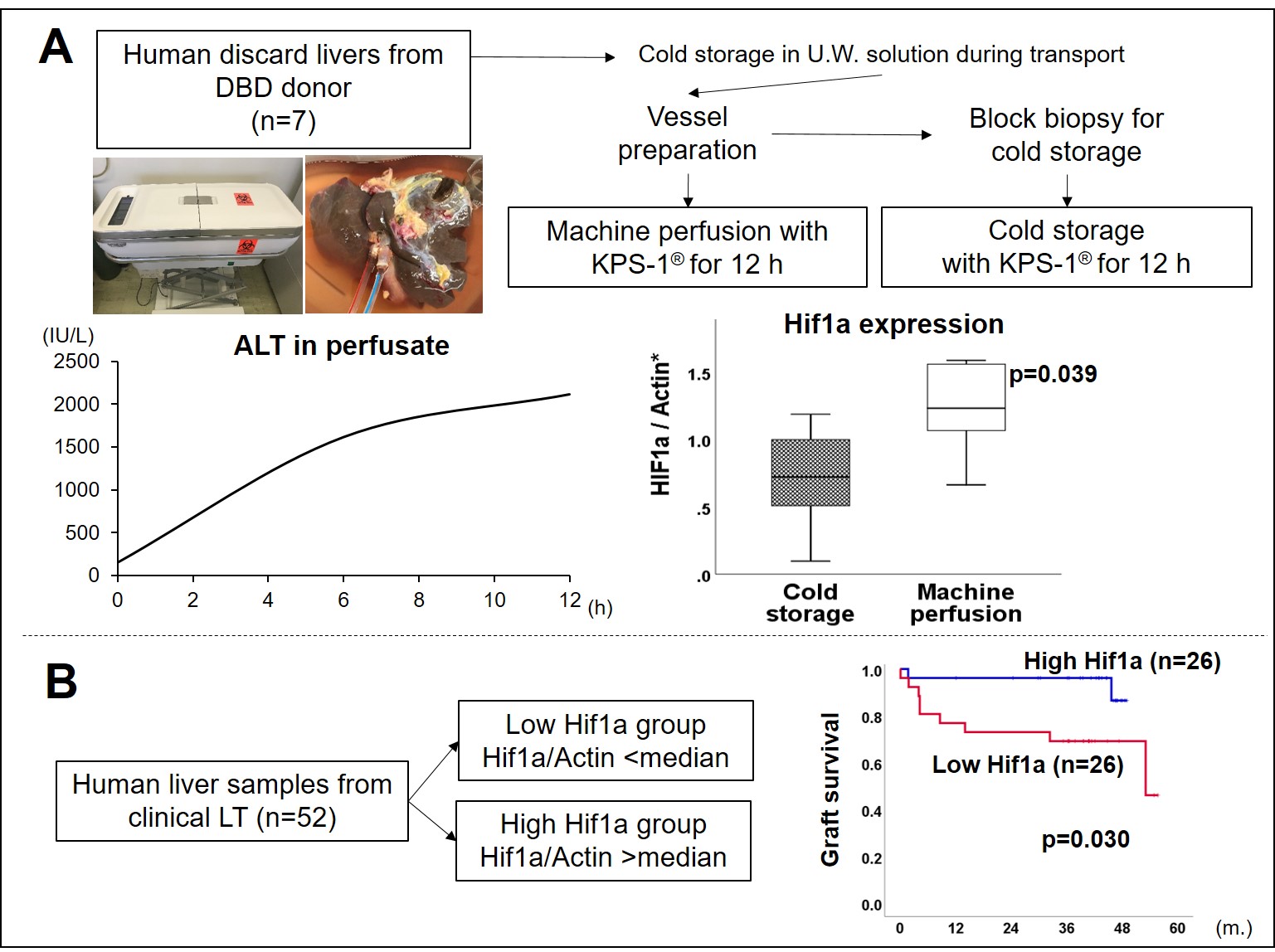
*Methods: From Oct. 2017 to Jan. 2019, seven human discarded livers from DBD donors underwent HMP. These livers were stored in cold University of Wisconsin (U.W.) solution during transport. Before connecting livers to machine, block biopsies from livers were obtained and they were cold stored in same solution for HMP to be used as static storage controls. LifePort® Liver Transporter System and KPS-1® solution were used for HMP. HMP was performed for 12 hours. Liver tissue and perfusate solution were collected. Pump flow rate was held constant. Hif1a expression was analyzed by PCR in the HMP and static storage tissue. In addition, its expression was assessed in transplanted grafts.
*Results: Among the 7 livers, 4 were declined by all centers due to steatosis (large droplet cells > 60%) and 3 due to unsuitable vessel quality. Median donor age / BMI were 52 years / 30.6 kg/m2, respectively. Median cold storage time before HMP was 737 (402-1105) min. There were no differences in histological staining by H.E. between the HMP livers and cold stored block biopsy tissue from the same livers. However, Hif1a expression by PCR in HMP livers after 12 h was significantly higher than that in cold stored tissue (figure A). To confirm the clinical impact of Hif1a, we assessed Hif1a expression in the liver before LT in 52 clinical LT patients. Grafts with high Hif1a expression had significantly superior survival compared to grafts with low Hif1a expression by median split (p=0.030, figure B).
*Conclusions: This is the first study demonstrating the impact of HMP on Hif1a expression in human livers. Hypothermic dynamic storage alone may potentially improve tolerance to hypoxia in human liver grafts. Further studies are warranted to clarify the detailed mechanism and clinical impact.
To cite this abstract in AMA style:
Ito T, Kadono K, Kojima H, Kageyama S, HIrao H, Nakamura K, Dery KJ, Murray AE, Aziz J, Busuttil RW, Kupiec-Weglinski J, Kaldas FM. Hypothermic Machine Perfusion Can Improve Hypoxia Tolerance in Human Discarded Liver [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/hypothermic-machine-perfusion-can-improve-hypoxia-tolerance-in-human-discarded-liver/. Accessed March 6, 2026.« Back to 2020 American Transplant Congress