High Level Cytomegalovirus Viremia in Liver Transplant Recipients: Risk Factors and Associated Outcomes
H. L. Kleiboeker1, M. R. Jorgenson1, G. E. Leverson2, J. P. Rice3, C. M. Saddler4, J. A. Smith4, D. Al-Adra3
1Pharmacy, University of Wisconsin Hospital and Clinics, Madison, WI, 2Department of Surgery, UW School of Medicine and Public Health, Madison, WI, 3Department of Medicine, Division of Gastroenterology and Hepatology, University of Wisconsin School of Medicine and Public Health, Madison, WI, 4Department of Medicine, Division of Infectious Diseases, University of Wisconsin School of Medicine and Public Health, Madison, WI
Meeting: 2022 American Transplant Congress
Abstract number: 1341
Keywords: Graft survival
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis) III
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: To evaluate epidemiology, risk-factors and outcomes of high-level CMV viremia in LTX recipients.
*Methods: Retrospective review of adults who received LTX between 1/1/2017-9/30/2020. Inclusion criteria required use of UW labs to allow for comparable viral loads. Primary objective was to describe incidence and outcomes of high-level (HL) CMV viremia (VL >100,000 IU/mL) after LTX. Secondary objective was to elucidate risk factors.
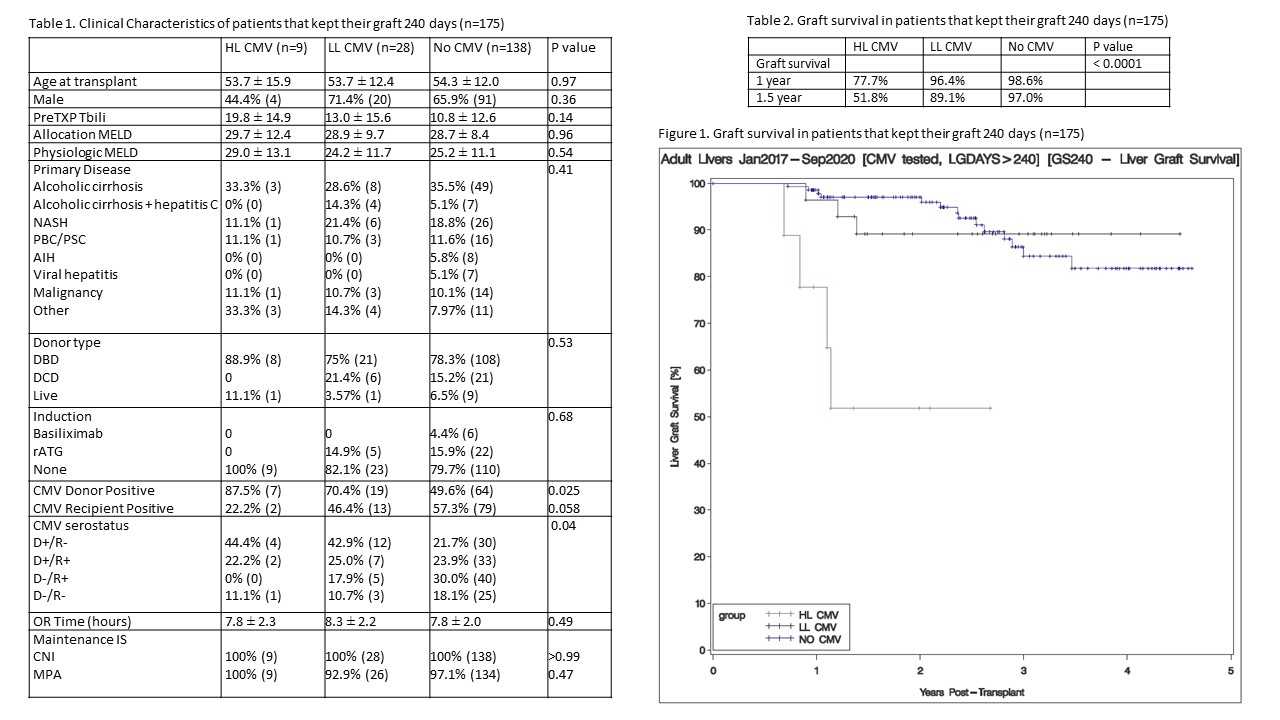
*Results: There were 209 patients that met inclusion criteria; 175 kept their graft for >240 days. Nine patients developed HL CMV , 28 experienced low-level CMV (LL CMV, VL 250-100,000 IU/mL) and 138 did not develop CMV viremia. Clinical characteristics found in Table 1. Time from transplant to CMV was 158 ± 77 days in HL CMV group and 150 ± 76 days in LL CMV group. Based on methods of Kaplan-Meier HL CMV was significantly associated with graft loss (p<0.0001). In additional analyses of the 209 transplants using time varying covariate models to assess the risk of developing HL CMV on subsequent liver graft loss, HL CMV appeared to be a negative outcome driver with significantly increased risk of graft loss (HR 5.6, p=0.0016). When investigating risk factors associated with HL CMV, donor seropositivity significantly increased risk (HR 8.85, 95% CI 1.13-71.43, p=0.038) with recipient seronegativity (HR 2.0, 95% CI 0.595-6.945, p=0.26), and pre-transplant total bilirubin (HR 1.0, 95% CI 0.998-1.07, p=0.06) possibly trending. Primary liver disease (p=0.92), clinical/allocation MELD (p=0.17, p=0.46), transplant surgery duration (p=0.73), age (p=0.68), sex (p=0.22), induction (p=0.99) and maintenance immunosuppression (p=0.99) were not significantly associated with development of HL CMV.
*Conclusions: While HL CMV after LTX is uncommon, it is associated with significantly increased risk of graft loss that is not present in patients who develop LL CMV. Given these negative graft effects, CMV stewardship interventions targeting recipients of CMV seropositive allografts are warranted. Future larger scale studies evaluating the potential role of recipient seronegativity and pre-transplant bilirubin in risk stratification are needed.
To cite this abstract in AMA style:
Kleiboeker HL, Jorgenson MR, Leverson GE, Rice JP, Saddler CM, Smith JA, Al-Adra D. High Level Cytomegalovirus Viremia in Liver Transplant Recipients: Risk Factors and Associated Outcomes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/high-level-cytomegalovirus-viremia-in-liver-transplant-recipients-risk-factors-and-associated-outcomes/. Accessed July 18, 2025.« Back to 2022 American Transplant Congress