High Incidence Of Anti-HLA DSA And Late Allograft Dysfunction In Solid Organ Transplant Recipients Hospitalized With Covid-19
University of Alabama at Birmingham, Birmingham, AL
Meeting: 2022 American Transplant Congress
Abstract number: 9029
Keywords: COVID-19, Graft function, HLA antibodies, Kidney transplantation
Topic: Basic & Clinical Science » Basic & Clinical Science » 73 - COVID-19
Session Information
Session Name: Late Breaking: Basic / Translational
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:40pm-4:50pm
Presentation Time: 4:40pm-4:50pm
Location: Hynes Room 313
*Purpose: Solid organ transplant (SOT) recipients admitted for COVID-19 commonly experience immunosuppression reduction and acute allograft dysfunction. Given the number of SOT patients hospitalized for COVID-19, it is critical to understand the natural history of alloimmunity and allograft dysfunction in this population.
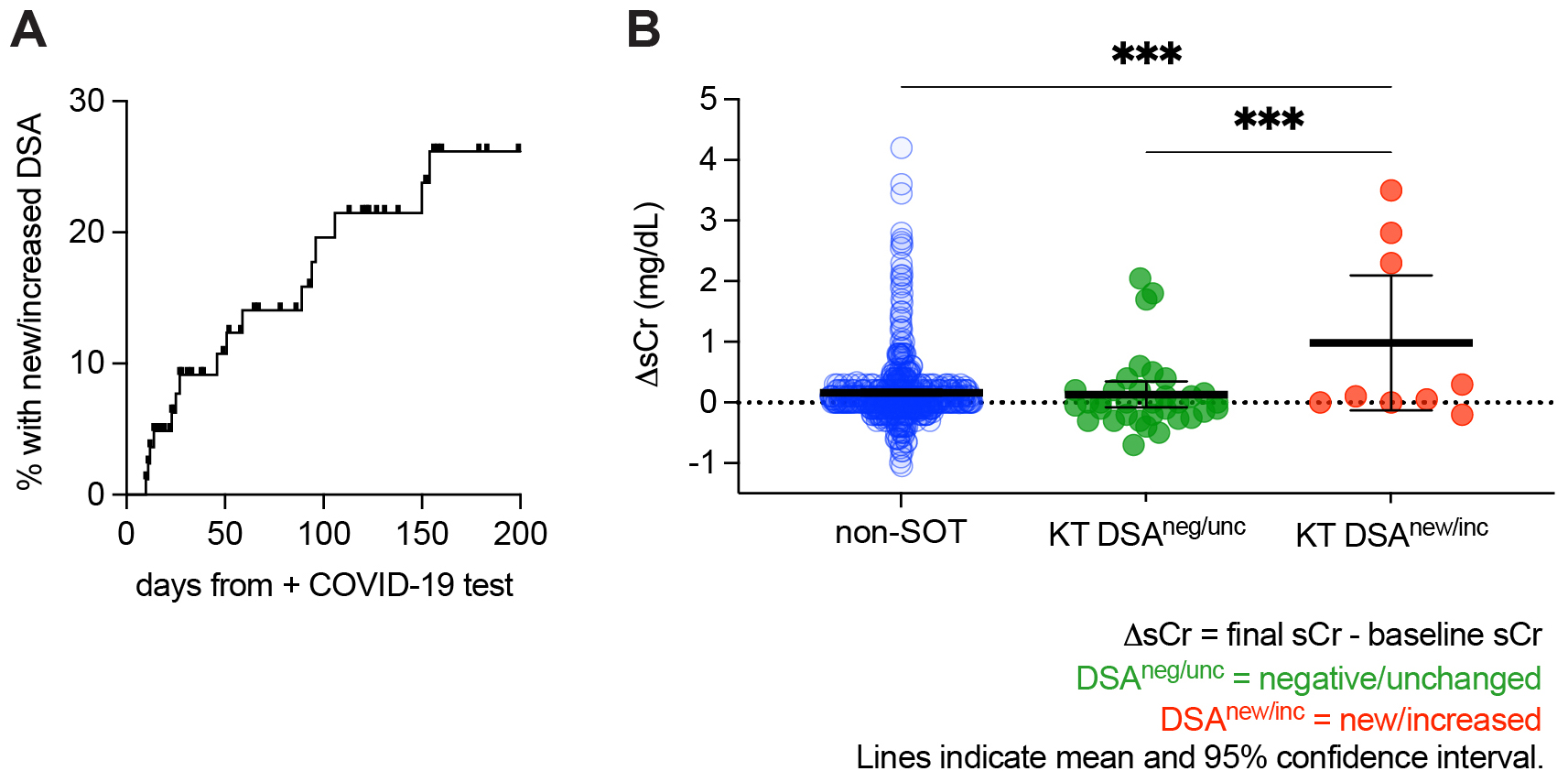
*Methods: We prospectively enrolled SOT patients admitted with COVID-19 to our institution between January 1, 2020 and June 1, 2021 as well as a non-SOT control cohort. We collected anti-HLA antibody (HLA-Ab) and renal function data. We retrospectively reviewed donor-specific antibody (DSA) assignments in the context of each patient’s transplant history and HLA typing. DSA that crossed the 1500 MFI threshold was classified as new DSA, and DSA that increased >1000 MFI was classified as increased DSA. For kidney transplant (KT) patients, we additionally evaluated renal function. The outcome of interest was change in serum creatinine (sCr) from pre-infection baseline to the most recent post-infection value. Baseline sCr was calculated as the median sCr in the year prior to COVID-19. For follow-up, the final sCr at least 60 days from COVID-19 was used. If the patient experienced allograft failure or the final sCr was >5.0 mg/dL, the final sCr was set equal to 5.0 mg/dL. Cumulative incidence of new or increased DSA was modeled with the Kaplan-Meier (KM) method. Group means were compared with one-way ANOVA using Tukey’s multiple comparisons test.
*Results: We enrolled 129 hospitalized SOT patients: 82 (64%) with a KT, 27 with a liver transplant, and the remainder with a heart, lung, or pancreas transplant. Of the 86 patients who underwent HLA-Ab testing 10-180 days after COVID-19 diagnosis, 15 developed new or increased DSA (Fig. 1A). We then evaluated the 39 KT patients with HLA-Ab testing, a baseline sCr, and a late sCr measurement. At a median follow-up of 330 days, KT patients with new or increased DSA (in red, Fig. 1B) showed a significantly greater increase in late sCr than both non-SOT patients (in blue) and KT patients without new or increased DSA (in green).
*Conclusions: New or increased DSA following hospitalization for COVID-19 is common in SOT patients, with a KM-estimated incidence of 25% in the six months following COVID-19. In KT patients, this DSA is associated with poorer allograft function. These data suggest a role for more intensive surveillance in SOT patients convalescing from COVID-19. Further studies will be needed to elucidate the contribution of infection, immunosuppression, and other factors.
To cite this abstract in AMA style:
Killian JT, Soto SRoman, Hauptfeld-Dolejsek V, Levitan EB, Porrett PM, Kumar V, Lund FE, Houp JA. High Incidence Of Anti-HLA DSA And Late Allograft Dysfunction In Solid Organ Transplant Recipients Hospitalized With Covid-19 [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/high-incidence-of-anti-hla-dsa-and-late-allograft-dysfunction-in-solid-organ-transplant-recipients-hospitalized-with-covid-19/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress