Functional Dependence, Access to Kidney Transplantation and Waitlist Mortality
1JHU, Baltimore, MD, 2UM, Ann Habor, MI
Meeting: 2019 American Transplant Congress
Abstract number: B52
Keywords: Age factors, Graft function, Resource utilization
Session Information
Session Name: Poster Session B: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Among patients with ESRD, functional dependence is common and an important determinant of both HRQOL and adverse outcomes. Kidney transplant (KT) may help patients with functional dependence regain their independence, an important patient-centered outcome. However, functional dependence are likely common in KT candidates and may also be associated with waitlist mortality and with delays in access to KT.
*Methods: We prospectively studied 3,987 patients being evaluated for KT at Johns Hopkins Hospital and University of Michigan (1/2009 and 6/2018). Functional dependence was determined by participant self-report of six Activities of Daily Living (ADL) domains (needing help with feeding, dressing, ambulation, grooming, using a toilet, and bathing) and eight IADL domains (needing help with using a phone, shopping, cooking, housework, washing, using transportation, managing medications, and managing money). We observed the cohort for a median of 38 (IQR 16-82) months from the time of KT evaluation to active listing, and from time of listing to waitlist mortality and KT. We used multivariable Cox regression to estimate the time-to-event of interest according to ADL/IADL disability.
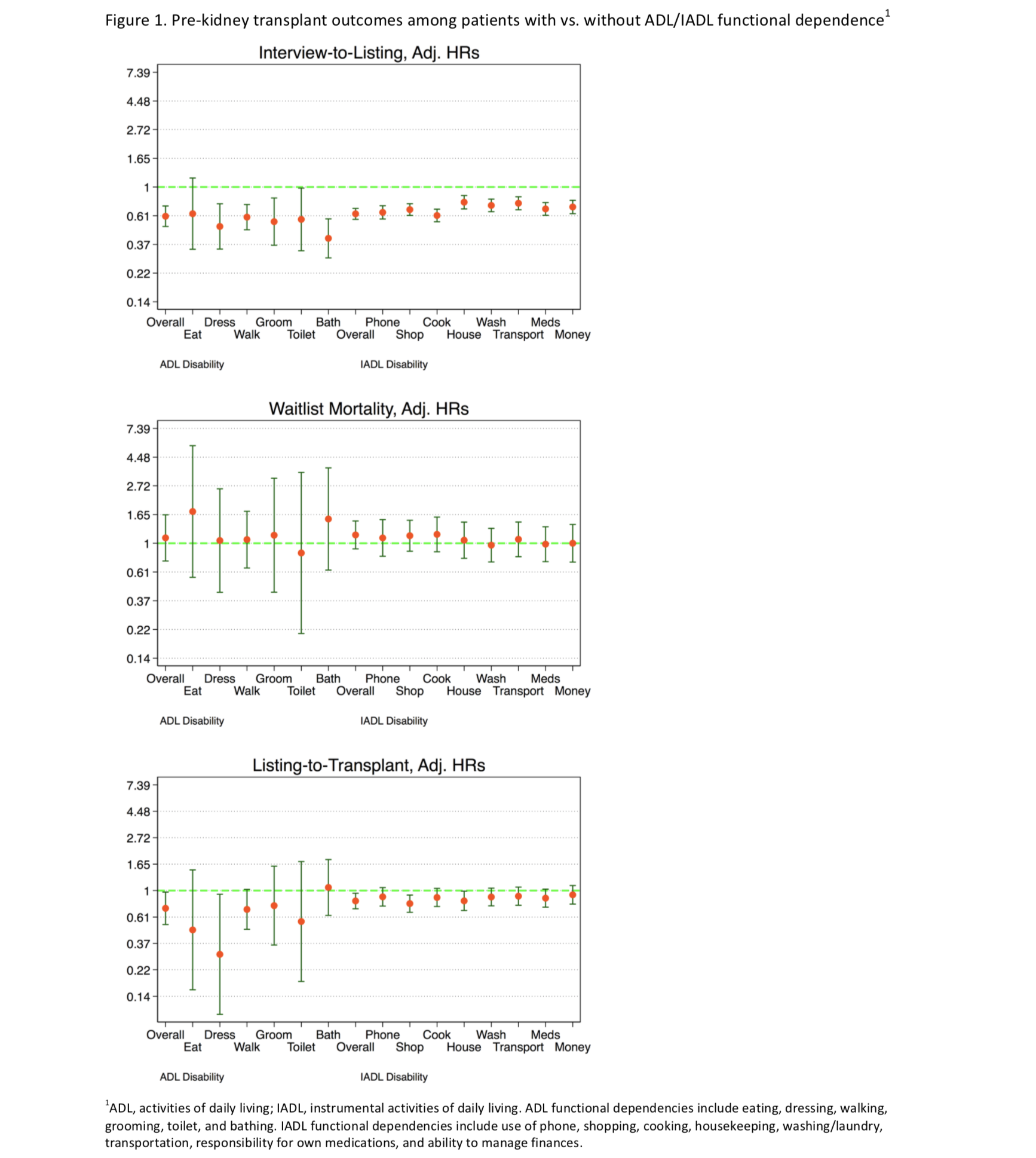
*Results: The median age of participants was 56 (IQR: 45-65) years and was higher among those with an ADL or IADL dependence (Table 1). The prevalence of functional dependence based on ADLs and IADLs was 8.6% and 30.4%, respectively. Of patients classified as having ADL dependence, 74% also had IADL dependence. Of those with IADL dependence, 21% had ADL dependence. After adjusting for age, sex, race, education, and diabetes, ADL and IADL were associated with lower chance of listing (ADL: hazard ratio [HR] 0.60, 95%CI 0.50-0.72, p<0.001; IADL: HR=0.63, 95%CI 0.57-0.69; p<0.001) and transplantation (ADL: HR 0.72, 95%CI 0.53-0.97, p=0.03; IADL: HR=0.82, 95%CI 0.71-0.95, p=0.008), but not waitlist mortality (ADL: HR=1.10, 95%CI 0.74-1.64, p=0.6; IADL HR=1.16, 95%CI 0.91-1.47, p=0.2). Similar associations were seen with the individual components of ADLs and IADLs in separate and same models but with varying degrees of statistical significance (Figure 1).
*Conclusions: Functional dependence based on ADLs and IADLs were common among patients undergoing evaluation for KT. Although they were associated with delays in listing and transplantation, these delays did not lead to increased waitlist mortality. This information may be used in discussions with patients with functional dependencies.
To cite this abstract in AMA style:
Muzaale A, Chu N, Ying H, Norman S, Sison S, Segev D, McAdams-Demarco M. Functional Dependence, Access to Kidney Transplantation and Waitlist Mortality [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/functional-dependence-access-to-kidney-transplantation-and-waitlist-mortality/. Accessed March 7, 2026.« Back to 2019 American Transplant Congress