Financial Impact of Testing Standardization for Solid Organ Transplant Recipients
1Division of Cardiology, University of Utah Health, Salt Lake City, UT
2Transplant Service Line, University of Utah Health, Salt Lake City, UT.
Meeting: 2018 American Transplant Congress
Abstract number: A377
Keywords: Cytomeglovirus, Economics, Heart transplant patients, Liver transplantation
Session Information
Session Name: Poster Session A: Quality Assurance Process Improvement
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Infection and bone marrow suppression surveillance is common practice in transplant recipients. Ordering of inappropriate lab tests can lead to repetitive blood draws, higher cost, and potential patient dissatisfaction. Protocols standardizing order sets and staff and patient education could result in achieving more cost-effective patient care.
Methods: In 2016, we implemented a protocol to reduce sources of variability in monitoring the complete blood count (CBC) and cytomegalovirus (CMV) infection status. We designated CBC with auto diff ($23.80) compared to CBC with platelets ($36.80) and CMV- Quantitative PCR ($310) compared to CMV-PCR ($374), as the preferred tests which would provide the necessary data for the routine patient surveillance at a lower cost. CBC with auto diff and CMV-Quantitative PCR were included in a standardized order set. Appropriate patient and staff education was also completed. The proportion of inappropriate tests and associated costs were compared between the pre- and post-protocol periods.
Results: There were 1,532 CMV tests performed among all solid organ transplant recipients, of which 692 (45%) were ordered before and 840 (55%) after the standardized protocol implementation. After protocol implementation, there was a 6.6% reduction in inappropriate CMV testing across all organs (P<0.001), which resulted in savings of $3,566 in the first year. There were 11,231 CBC tests performed, 6,201 before and 5,030 after protocol implementation. In heart transplant recipients, there was a significant decline in the number of inappropriate tests after protocol implementation 26.2% to 20.3%, p=0.04, which resulted in $300 savings in the first year. 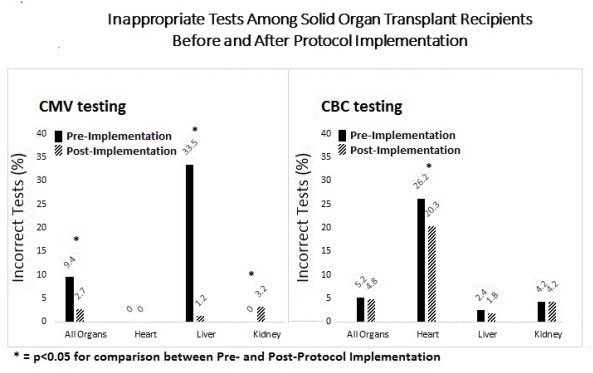
Conclusion: Standardization of post-transplant testing in solid organ transplant recipients resulted in reduced costs while providing the necessary surveillance data. Further work is needed to achieve higher level of adherence to per-protocol test ordering.
CITATION INFORMATION: Ugolini S., Dranow L., Sadler P., Berry M., Stehlik J., Drakos S., Nativi J., Gilbert E., McKeller S., Koliopoulou A., Yin M., Davis E., Selzman C., Wever-Pinzon O. Financial Impact of Testing Standardization for Solid Organ Transplant Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ugolini S, Dranow L, Sadler P, Berry M, Stehlik J, Drakos S, Nativi J, Gilbert E, McKeller S, Koliopoulou A, Yin M, Davis E, Selzman C, Wever-Pinzon O. Financial Impact of Testing Standardization for Solid Organ Transplant Recipients [abstract]. https://atcmeetingabstracts.com/abstract/financial-impact-of-testing-standardization-for-solid-organ-transplant-recipients/. Accessed March 7, 2026.« Back to 2018 American Transplant Congress
