Extracorporeal Membrane Oxygenation in Pediatric Liver Transplantation
1Vanderbilt University Medical Center, Nashville, TN, 2Children's Hospital Association, Lenexa, KS, 3Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN
Meeting: 2020 American Transplant Congress
Abstract number: C-176
Keywords: Graft survival, Liver transplantation, N/A, Pediatric
Session Information
Session Name: Poster Session C: Liver: Pediatrics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Extracorporeal membrane oxygenation (ECMO) can be used for oxygen preservation and hemodynamic support in case of circulatory or respiratory failure. Although the role of ECMO has emerged in the setting of adult liver transplantation (LT), data in children are limited. We aimed to describe the frequency of ECMO use following LT in children and report the post-LT outcomes.
*Methods: All pediatric LT recipients requiring ECMO support post-LT were identified from a linked Pediatric Health Information System/Scientific Registry of Transplant Recipients dataset (2003-2018). Patient demographics were described with summary statistics and survival rates were compared with the log-rank test.
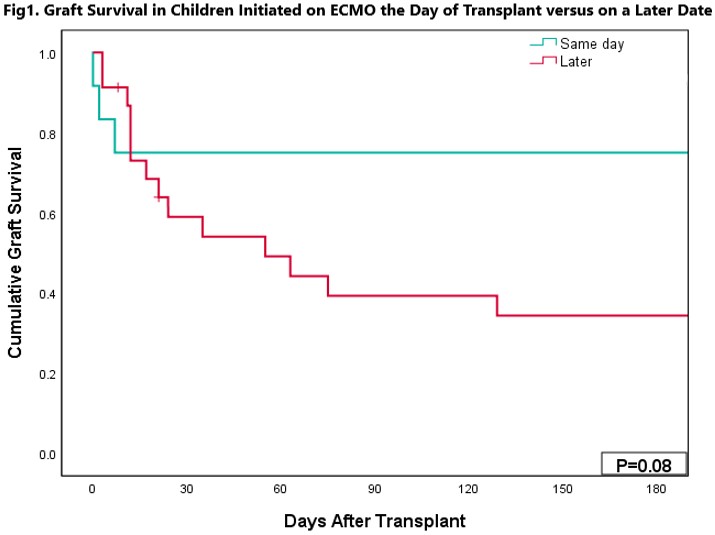
*Results: 35 children (3 living, 32 deceased donor LT) with a median age of 4 (range 0-20) years were included. 45.7% were female (n=16/35) and the primary listing diagnoses were most commonly acute liver failure (22.9%; n=8/35), tumor (20%; n=7/35), cholestatic liver disease (20%; n=7/35) and cirrhosis (14.3%; n=5/35). History of heart failure was reported in 6 patients (17.1%), hepatopulmonary syndrome in 5 (14.3%) and pulmonary artery anomaly in 4 (11.4%). The median time from LT to ECMO initiation was 4 (IQR: 0-12) days and the median ECMO duration was 1 (IQR: 1-6) days. 6 patients (17.1%) required in-hospital dialysis, 21 in-hospital resuscitation (60%) and 16 (45.7%) in-hospital mortalities were reported. Cause of death was of cardiac etiology in 25% (n=4/16), multiorgan failure in 25% (n=4/16), graft failure, respiratory failure, and hemorrhage each in 12.5% (n=2/16), infection and unknown each in 6.3% (n=1/16). Children initiated on ECMO the day of LT had a tendency for superior patient and graft survival compared to those started on ECMO on a later date (P=0.13 and P=0.08 [Fig.1], respectively). The 6-month patient and graft survival rates were 75% and 75% for those started on ECMO on the day of LT compared to 39% and 34% for those started on ECMO on a later date. Length of hospital stay was 41 (IQR: 20-69) days. ECMO use in pediatric LT has increased over time (R2 Linear=0.23, P=0.06).
*Conclusions: This study highlights the feasibility of ECMO to provide cardiopulmonary support in pediatric LT recipients. With >54% patient survival, ECMO should not be considered a futile modality and should be initiated early. The indications and cannulation strategy for ECMO in pediatric LT merit further investigation.
To cite this abstract in AMA style:
Ziogas IA, Johnson WR, Thurm C, Hall M, Matsuoka LK, Montenovo MI, Bacchetta MD, Godown J, Alexopoulos SP. Extracorporeal Membrane Oxygenation in Pediatric Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/extracorporeal-membrane-oxygenation-in-pediatric-liver-transplantation/. Accessed March 8, 2026.« Back to 2020 American Transplant Congress