Effect of DSA-Free Heart Allocation
1University of Michigan, Ann Arbor, MI, 2SRTR, Minneapolis, MN, 3UT Southwestern, Dallas, TX
Meeting: 2020 American Transplant Congress
Abstract number: 293
Keywords: Donation, Efficacy, Graft acceptance, Waiting lists
Session Information
Session Name: Heart Transplantation: Allocation, Allocation, Allocation
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Virtual
*Purpose: Currently, donation service area (DSA) is the first geographic unit for heart allocation, which creates discrepancies in access for high-urgency candidates. We studied the effect of replacing DSA with distance circles of varying radii.
*Methods: Thoracic simulated allocation model (TSAM) software and OPTN data were used to simulate the effects of four DSA-free allocation rules on transplant, waitlist mortality, and 1-year posttransplant mortality rates. The four allocation rules were: 150 nautical miles (NM) from donor to recipient hospitals, 250NM, 500NM-A (broader sharing to 1000NM for status 1 and 2 candidates), and 500NM-B (without broader sharing). The study included 9913 adult heart transplant candidates listed for at least 1 day from June 30, 2009, to June 30, 2011. Each simulation was repeated 10 times with different orderings of organ arrivals to provide a measure of variability. Comparisons were made to DSA-first allocation.
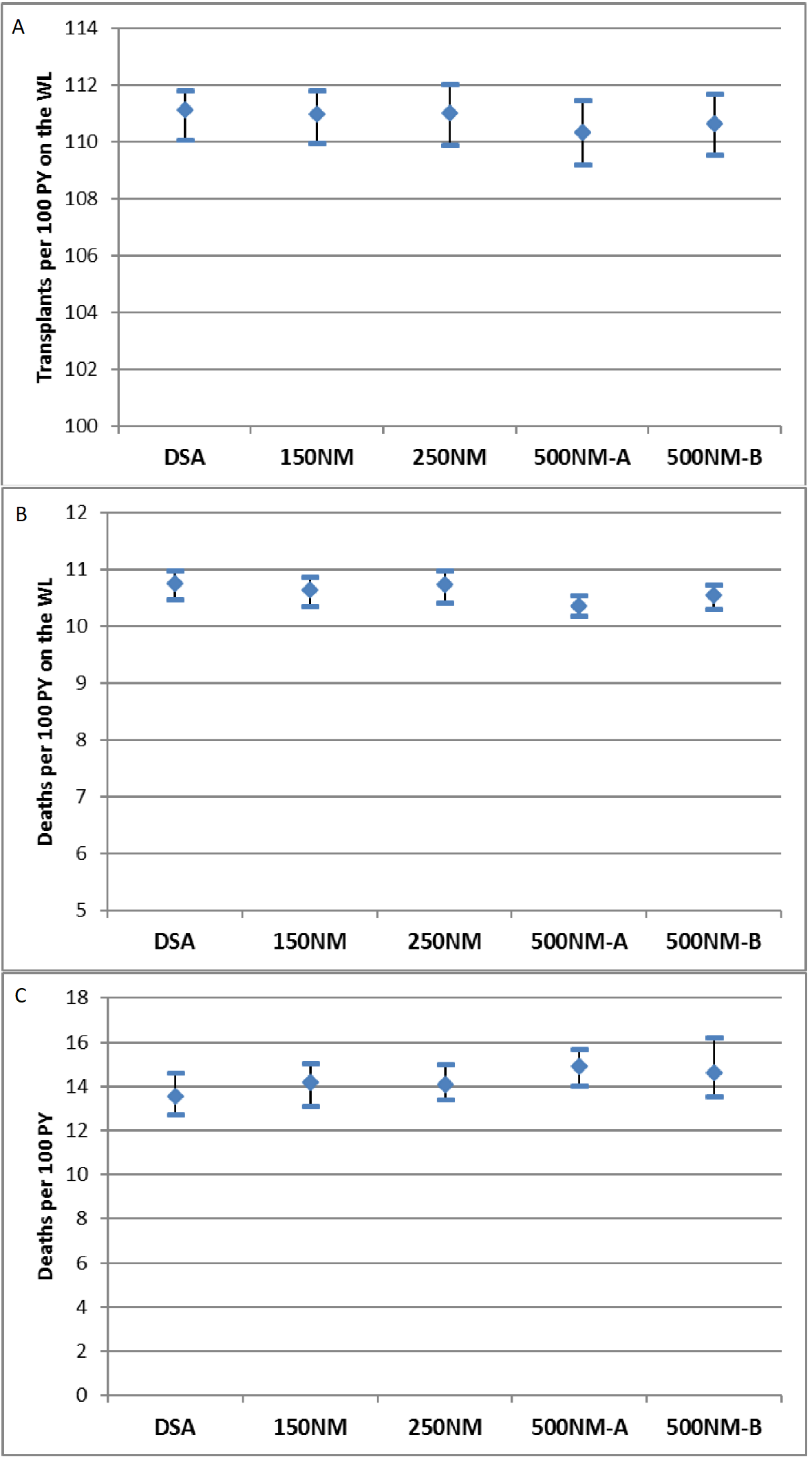
*Results: Compared with DSA-first allocation, DSA-free rules had little impact on overall transplant, waitlist mortality, or 1-year posttransplant mortality rates (Figures 1a-1c). The median distance was lowest, 144NM, under the 150NM rule, and highest, 346NM, under 500NM-A. For status 1 and 2 candidates, transplant rates were higher in the 500NM-A simulation compared with DSA-first, while for status 4 candidates, rates decreased in the 250NM, 500NM-A, and -B simulations. For the other statuses, transplant rates were similar across the simulations. Waitlist mortality and 1-year posttransplant mortality were similar across all simulations for all statuses. Transplant rates and counts in all DSA-free simulations were similar to the DSA-first simulation in most regions. In OPTN regions 1 and 9, transplant rates increased under the 500NM-A and 500NM-B rules compared with DSA-first. In OPTN region 2, transplant rates decreased under 150NM, 250NM, and 500NM-B. Waitlist and posttransplant mortality in OPTN regions was similar across allocation rules except for decreased mortality in region 1 under 500NM-A.
*Conclusions: In general, simulations showed little overall difference in waitlist and posttransplant outcomes under DSA-first vs. DSA-free allocation rules despite slight regional variations in transplant rates and a decrease in transplant rate for status 4 under 500NM-A. We conclude, based on allocation simulation, that elimination of DSAs may increase access to transplant for the highest urgency categories without significantly impacting post-transplant and waitlist mortality.
To cite this abstract in AMA style:
Patel V, Skeans M, Cascino T, Davies R, Colvin M. Effect of DSA-Free Heart Allocation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/effect-of-dsa-free-heart-allocation/. Accessed February 26, 2026.« Back to 2020 American Transplant Congress