Early Relapse of Atypical HUS Following ABO Incompatible Living Related Paediatric Renal Re-Transplant Successfully Treated With Eculizumab
1Department of Paediatric Nephrology, Great Ormond Street Hospital NHS Foundation Trust, London, United Kingdom
2Department of Transplantation, Guy's and St Thomas'
NHS Foundation Trust, London, United Kingdom
3Department of Histopathology, Great Ormond Street Hospital NHS Foundation Trust, London, United Kingdom.
Meeting: 2015 American Transplant Congress
Abstract number: D221
Keywords: Graft survival, Kidney transplantation, Pediatric, Recurrence
Session Information
Session Name: Poster Session D: Pediatric Clinical Kidney Transplantation
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background. The female patient presented at 3 years of age with clinical features suggestive of aHUS confirmed genetically as complement factor I mutation (heterozygous for CFI c.1216C>T,p.(Arg406Cys) in patient and asymptomatic mother. Patient also had antibodies to complement factor H. She was initially treated with 37 plasma exchange sessions,progressed to ESKD and commenced dialysis. She was unsuccessful in 5 runs of national living donor kidney sharing scheme. She received en bloc DCD transplant (paediatric donor) which failed to perfuse and was removed at time of transplantation.
Methods. Prospective case study.
Results. Patient received an ABOi live related kidney transplant from father at 9 years using quadruple immunosuppression (basiliximab, mycophenolate mofetil, tacrolimus, corticosteroids) with B lymphocyte depletion (rituximab 375mg/m2).Recipient and donor blood groups were O and A respectively with anti-A titres of 1:128. Four sessions of immunoadsorption reduced anti-A titres to 1:4 at time of transplant. Six hours post-transplant,she had of recurrence of aHUS:allograft dysfunction, rising LDH, dropping haemoglobin and thrombocytopenia. She received 1st dose of eculizumab within hours and 2nd dose the next day. Histology confirmed thrombotic microangiopathy(TMA). Allograft function improved and patient currently receives monthly eculizumab. We measured eculizumab levels at peak (420.5 ug/mL), at 2 weeks (273.8 ug/mL) and 3 weeks (246.4 ug/mL) after infusion. One year after the transplant, she has stable allograft function with eGFR of 66mls/min/1.73m2, EBV and BK viraemia, normal LDH, haemoglobin and platelets; negative anti-A titres and no evidence of TMA on biopsy.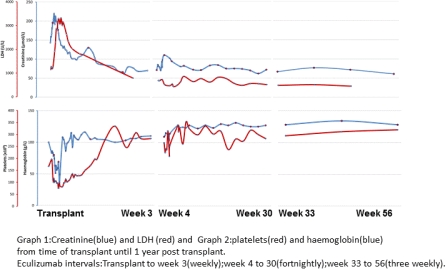
Conclusion. This is the first report of a paediatric ABOi living related renal transplantation in whom early relapse of aHUS was successfully treated with eculizumab.
To cite this abstract in AMA style:
Stojanovic J, Adamusiak A, Sebire N, Marks S, Mamode N. Early Relapse of Atypical HUS Following ABO Incompatible Living Related Paediatric Renal Re-Transplant Successfully Treated With Eculizumab [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/early-relapse-of-atypical-hus-following-abo-incompatible-living-related-paediatric-renal-re-transplant-successfully-treated-with-eculizumab/. Accessed July 12, 2025.« Back to 2015 American Transplant Congress
