Early Allograft Dysfunction as a Predictor for Graft and Patient Survival after Liver Transplantation
Multi Organ Transplant Program, Toronto General Hospital, Toronto, ON, Canada
Meeting: 2020 American Transplant Congress
Abstract number: B-154
Keywords: Graft survival, Liver transplantation, Survival
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
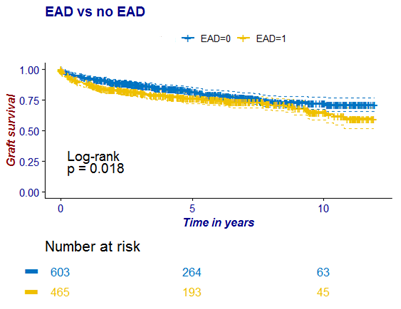
*Purpose: Early allograft dysfunction (EAD) after liver transplantation has been associated with long-term reduced graft and patient survival. In this single center cohort study, we aimed to compare incidence, risk factors and outcomes in liver transplant recipients who developed EAD.
*Methods: Patients who received donation after circulatory death (DCD) or donation after brain death (DBD) grafts between January 2007 and December 2017 were included. EAD was defined as a bilirubin of >10 (171μm/L) or an international normalised ratio of >1.6 on post-operative day 7 or transaminases >2000 U\l in the first week as previously described.
*Results: In our cohort of 1068 patients, incidence of EAD was 43.53%. EAD occurred more frequently in the DCD group (p<0.01). Recipients who developed EAD showed a significantly lower graft and patient survival at 1-, 3-, and 5-years after transplantation (all p<0.05). Univariate analysis revealed that recipient BMI and MELD score (p= 0.007, p=0.056), donor age, BMI and gender (p=0.006, p<0.001, p=0.01) and warm ischemia time, estimated blood loss, vasopressor necessity at one hour and the end of transplant and the amount of fresh frozen plasma that was administered (p<0.001, p=0.002, p=0.008, p=0.027 and respectively 9=0.045) were significantly different between groups. Subgroup analysis showed that for recipients of DBD grafts, predictive markers of EAD were donor age and BMI, recipient BMI, MELD score and HCV infection, warm ischemia time and cold ischemia time. For DCD recipients, donor BMI, catecholamine demand at the end of transplant and cold ischemia time were associated with EAD.
*Conclusions: In our cohort study, EAD resulted in poorer long-term patient and graft survival. Predictive markers for EAD are dependent on the donor type.
To cite this abstract in AMA style:
Mazilescu LI, Selzner N, Sapisochin G, Reichman T, Bhat M, Cattral M, Lilly L, McGilvray I, Galvin Z, Ghanekar A, Selzner M. Early Allograft Dysfunction as a Predictor for Graft and Patient Survival after Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/early-allograft-dysfunction-as-a-predictor-for-graft-and-patient-survival-after-liver-transplantation/. Accessed February 26, 2026.« Back to 2020 American Transplant Congress