Early Acute Cellular Rejection(eACR) as a Marker of Immunologic Competency Following Liver Transplantation(LT).
University of Minnesota, Minneapolis, MN
Meeting: 2017 American Transplant Congress
Abstract number: 253
Keywords: Infection, Liver transplantation, Malignancy, Rejection
Session Information
Session Name: Concurrent Session: Liver Retransplantation and Other Complications
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: E353B
Background:Historically eACR did not adversely impact patient survival(PS). Since infection(Ifx) is major cause of death(COD) among LT recipients, we hypothesized that eACR is marker of immunologic competence, resulting in fewer Ifx-and malignancy-related deaths. Methods:1385LT were performed,1983-2014. eACR was defined:0-3 months(Ms) by treatment/biopsy. Demographics, PS/DCGS were compared for 0,1,>1 eACR groups. Multivariable models were used to adjust for recipients characteristics. Cause of death(COD), cause of graft loss(CGL), Ifx(0-3 and 4-12Ms post-LT) were compared. Results:1256(91%) recipients survived past 3Ms; 1068(85%) had=0, 147(12%)=1 and 41(3%)>1 eACR; 80% were biopsy-proven. Younger age, female gender, lower BMI, deceased donor, biliary atresia, early Ifx were risk factors(RF) for eACR(P<0.01). Hazard of death was 0.60[CI:0.43-0.85] for recipients w/1 and 0.51[CI:0.28-0.9] for recipient w/>1 eACR(Figure 1A); there was no difference in DCGS(Figure 1B). Median PS for HCV recipients was 11vs.18yrs.(entire cohort);with eACR, median PS for HCV recipients was 9vs.12yrs. w/out eACR. Most common COD were Ifx and malignancy. Overall Ifx-COD was similar between groups(21-25%); bacterial(Ifx)-COD was 28%, 78%, 67%, for recipients with 0,1,>1 eACR groups(P<0.05). Overall malignancy deaths were 22%, 12%, 0%, for 0,1,>1 eACR groups(P<0.05); 81% occurred within 10yrs. post-LT(Figure 2A). Most common CGL were chronic rejection(CR) and HCV recurrence(HCV-R)(Figure 2B). (Ifx)rates, between 4-12M, ranged 11-15%.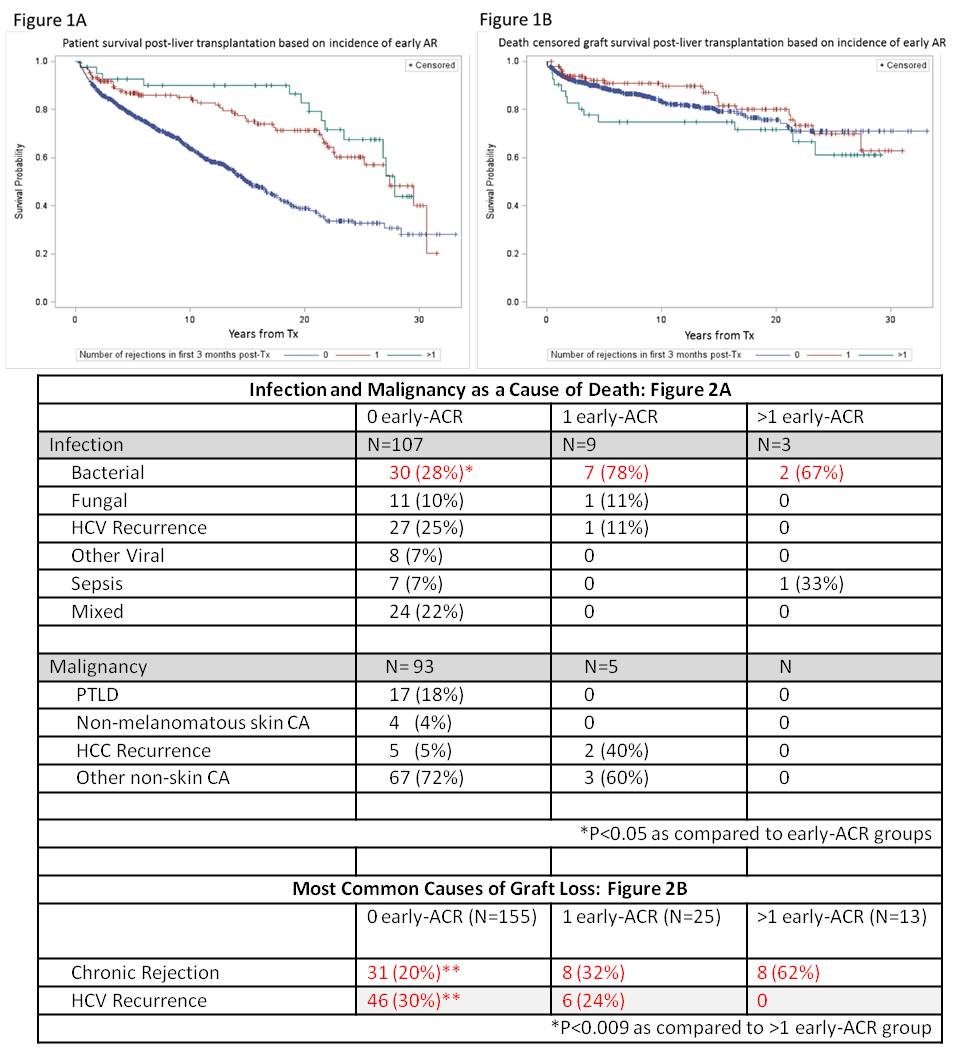 Conclusion:For entire cohort, presence of eACR is associated with improved PS but doesn't affect DCGS; for HCV subpopulation, eACR is associated with inferior PS. Although, recipients with eACR had lower rate of malignancy-related deaths,which may suggest immunological competence;their rate of death from bacterial(Ifx) was higher. eACR group(>1) lost more grafts to CR;recips. without eACR lost graft to HCV-R, which reflects non-uniform distribution of eACR among recips. with different liver disease etiologies.
Conclusion:For entire cohort, presence of eACR is associated with improved PS but doesn't affect DCGS; for HCV subpopulation, eACR is associated with inferior PS. Although, recipients with eACR had lower rate of malignancy-related deaths,which may suggest immunological competence;their rate of death from bacterial(Ifx) was higher. eACR group(>1) lost more grafts to CR;recips. without eACR lost graft to HCV-R, which reflects non-uniform distribution of eACR among recips. with different liver disease etiologies.
CITATION INFORMATION: Kirchner V, Bandgdiwala A, Vock D, Hassan M, Kandaswamy R, Lake J, Lim N, Mahgoub A, Minja E, Pugalenthi A, Sengupta B, Serrano O, Thompson J, Payne W, Pruett T, Chinnakotla S. Early Acute Cellular Rejection(eACR) as a Marker of Immunologic Competency Following Liver Transplantation(LT). Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Kirchner V, Bandgdiwala A, Vock D, Hassan M, Kandaswamy R, Lake J, Lim N, Mahgoub A, Minja E, Pugalenthi A, Sengupta B, Serrano O, Thompson J, Payne W, Pruett T, Chinnakotla S. Early Acute Cellular Rejection(eACR) as a Marker of Immunologic Competency Following Liver Transplantation(LT). [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/early-acute-cellular-rejectioneacr-as-a-marker-of-immunologic-competency-following-liver-transplantationlt/. Accessed February 28, 2026.« Back to 2017 American Transplant Congress
