Donor Specific Antibodies and Clinical Outcomes in Kidney Transplant Recipients
1Department of Renal Medicine, Royal Prince Alfred Hospital, Sydney, Australia
2Sydney Medical School, University of Sydney, Sydney, Australia.
Meeting: 2018 American Transplant Congress
Abstract number: D92
Keywords: Graft survival, HLA antibodies, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session D: Kidney Complications: Late Graft Failure
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
BACKGROUND: Donor specific antibodies (DSA) have been implicated in the development of acute rejection (AR) and graft dysfunction in kidney transplant recipients (KTx). However, limited data exists on their natural history after transplantation.
AIM: To describe the natural history of pre-transplant and denovo DSA (dnDSA) in KTx.
METHODS: We performed a prospective single centre cohort study in KTx. Patients were screened for DSA pre-transplant, 3 and 12 months post-transplant, and during graft dysfunction. The associations between DSA and outcomes were assessed using multivariable analysis.
RESULTS: 363 KTx between 2010–2017 underwent pre- and post-transplant DSA screening. Pre-transplant DSA (preDSA) were detected in 136 patients (37%) at transplantation, of whom 47 (34%) had Class I preDSA, 50 (37%) had Class II, and 39 (29%) had Class I and II. The median MFI of the dominant preDSA was 1230 (IQR 746-2528) at transplantation and declined rapidly, becoming undetectable by 30 days post-transplant. The burden of preDSA, defined as the total MFI for all preDSA for each patient, declined in the first month post-transplant and remained constant to month 12.
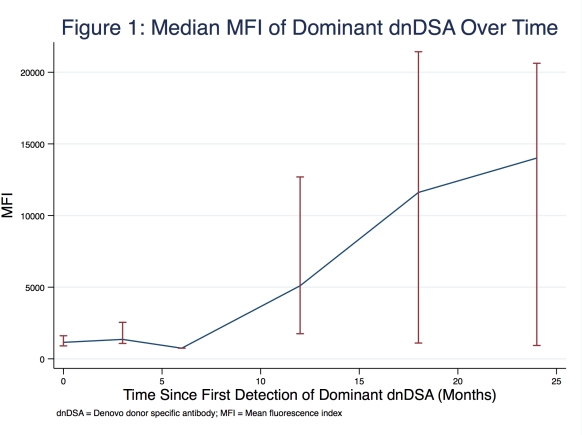
dnDSA were detected in 62 recipients (17%) of whom 17 (27%) had Class I dnDSA, 34 (55%) had Class II, and 11 (18%) had Class I and II. The median time to first detection of dnDSA was 58 days (IQR 15-267) and the median MFI of the dominant dnDSA was 1150 (IQR 707-2694) at the time of first detection. The MFI of the dominant dnDSA increased progressively over time reaching a median of 14,011 (IQR 931-20,626) at 2 years (Figure 1). 58 (26%) of 220 patients with at least 2 years of follow-up developed AR; 38 (17%) had cell mediated rejection, 16 (7%) had antibody mediated rejection, and 4 (2%) had mixed rejection. The development of dnDSA was strongly associated with AR (OR 4.48; 95%CI 2.14-9.36; P<0.001) but not with eGFR or death censored graft survival.
CONCLUSION: PreDSA were present in 37% of KTx and were significantly reduced by 1 month post-transplant. dnDSA were detected in 17% and increased in intensity over time. The development of dnDSA was strongly associated with AR.
CITATION INFORMATION: Wan S., Chadban S., Wyburn K. Donor Specific Antibodies and Clinical Outcomes in Kidney Transplant Recipients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Wan S, Chadban S, Wyburn K. Donor Specific Antibodies and Clinical Outcomes in Kidney Transplant Recipients [abstract]. https://atcmeetingabstracts.com/abstract/donor-specific-antibodies-and-clinical-outcomes-in-kidney-transplant-recipients/. Accessed February 25, 2026.« Back to 2018 American Transplant Congress