Donation After Cardiac Death (DCD) Liver Transplantation (LT) Is Not Associated with Post-LT Renal Dysfunction.
Transplant, Mayo Clinic, Jacksonville, FL
Meeting: 2017 American Transplant Congress
Abstract number: C189
Keywords: Donors, Liver transplantation, non-heart-beating, Renal function
Session Information
Session Name: Poster Session C: Organ Allocation, Meld Score, Organ Utilization, and Transplant Outcomes
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
The relationship between DCD LT and post-LT renal dysfunction is unclear. Aim: Determine the effects of DCD LT compared to donation after brain death (DBD) LT on post-LT renal outcomes including 1) renal function at 1, 4 and 12 month; 2) new onset acute kidney injury (AKI) requiring renal replacement therapy (RRT) in the 1st post-LT month and 3) end-stage renal disease (ESRD) at 1 year from LT. Methods: Data on 1325 (1157 DBD and 168 DCD) 1ry LT performed between January 2003 and December 2011 were retrospectively reviewed. Kidney function was assessed by serum creatinine (Cr) at 1, 4 and 12 months post-LT and 24-hr urine Cr clearance at 1 year. Rates of AKI requiring RRT within the 1st post-LT month and ESRD at 1 yr were recorded. Patient and graft survival were calculated using the Kaplan-Meier method and compared between DBD and DCD LT. Results: Patients' demographics and post-LT renal outcomes are summarized in Table 1.
| DBD (n=1157) | DCD (n=168) | P | |
| Age | 56±10 | 55.5 ± 9.6 | 0.8 |
| % Male | 67 | 73 | 0.1 |
| % Caucasian | 91 | 94 | 0.7 |
| %HCV | 38 | 49 | 0.005 |
| MELD score | 19±8 | 18±7 | 0.1 |
| Serum Cr at LT | 1.1±0.7 | 1.0±0.6 | 0.2 |
| Pre-LT 24-hr Cr clearance | 72±37 | 74±38 | 0.7 |
| %on RRT at LT | 5.7 | 6 | 0.9 |
| Renal Outcomes | |||
| %New AKI post-LT | 5.4 | 4.8 | 0.7 |
| %ESRD at 1 yr | 2.7 | 4.2 | 0.3 |
| 1 month Cr | 1.2±0.5 n=1124 | 1.2±0.5 n=161 | 0.9 |
| 4 month Cr | 1.3±0.6 n=1008 | 1.2±0.4 n=149 | 0.4 |
| 1 yr Cr | 1.2±0.5 n=873 | 1.2±0.4 n=133 | 0.3 |
| 1 yr 24 hr Cr clearance | 61±25 n=722 | 63±27 n=113 | 0.4 |
Patient and graft survivals were also similar between DBD and DCD LT (Figure 1).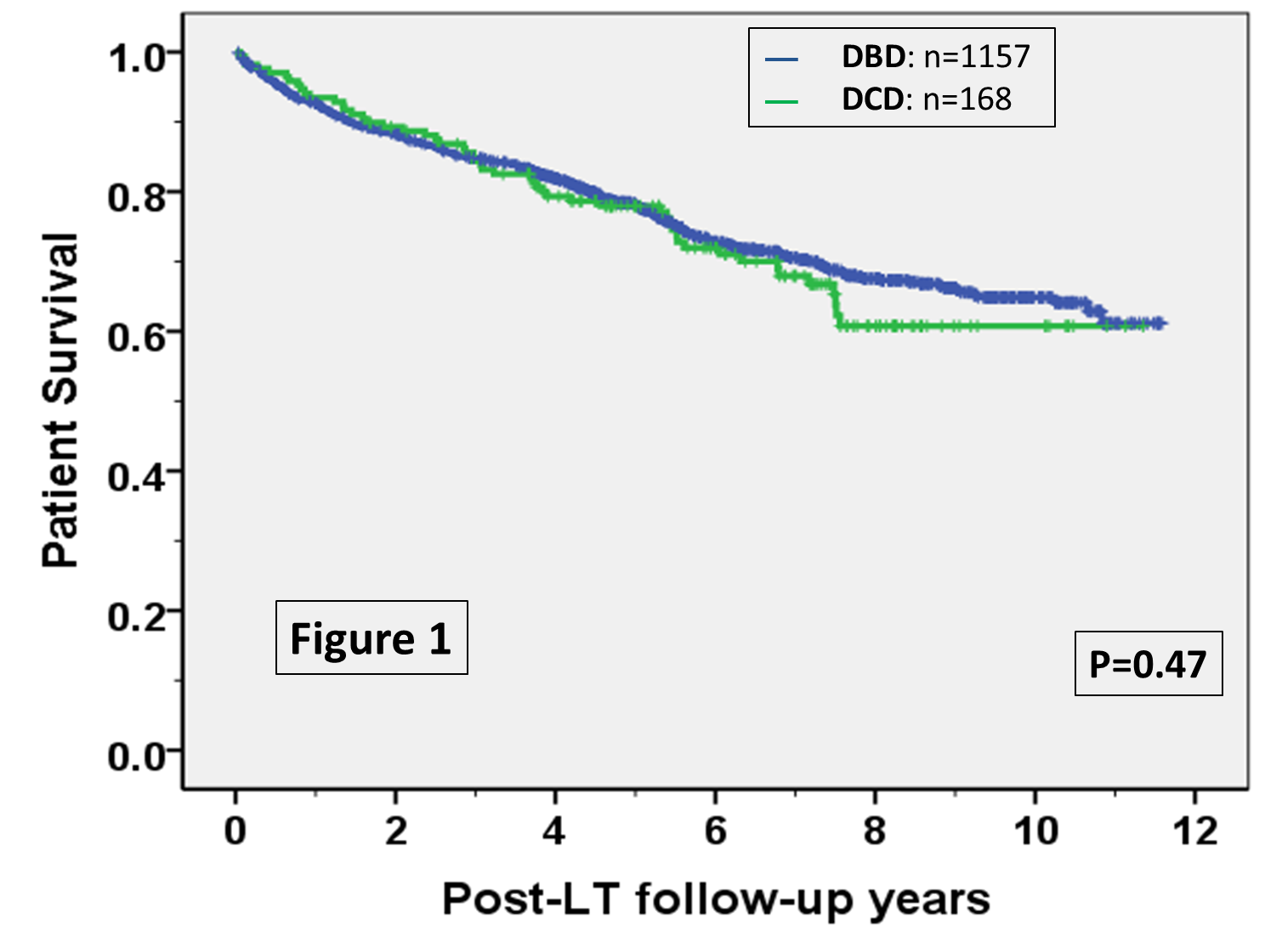 Conclusions: 1)DCD LT is not associated with increased risk of post-LT AKI requiring RRT within the 1st month post-LT or ESRD within the 1st year post-LT. 2)Serum Cr and Cr clearance were similar at 1, 4 and 12 months post-LT between DCD and DBD LT recipients.
Conclusions: 1)DCD LT is not associated with increased risk of post-LT AKI requiring RRT within the 1st month post-LT or ESRD within the 1st year post-LT. 2)Serum Cr and Cr clearance were similar at 1, 4 and 12 months post-LT between DCD and DBD LT recipients.
CITATION INFORMATION: Wadei H, Mai M, Lee D, Croome K, Rosser B, Keaveny A, Taner B. Donation After Cardiac Death (DCD) Liver Transplantation (LT) Is Not Associated with Post-LT Renal Dysfunction. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Wadei H, Mai M, Lee D, Croome K, Rosser B, Keaveny A, Taner B. Donation After Cardiac Death (DCD) Liver Transplantation (LT) Is Not Associated with Post-LT Renal Dysfunction. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/donation-after-cardiac-death-dcd-liver-transplantation-lt-is-not-associated-with-post-lt-renal-dysfunction/. Accessed February 20, 2026.« Back to 2017 American Transplant Congress
