Differential Impact of Subclinical Kidney Transplant Rejection in Young Adults
1School of Medicine, University of Alabama at Birmingham, Birmingham, AL, 2College of Medicine, University of Nebraska, Omaha, NE
Meeting: 2022 American Transplant Congress
Abstract number: 1543
Keywords: Age factors, Kidney transplantation, Outcome, Rejection
Topic: Basic Science » Basic Clinical Science » 17 - Biomarkers: Clinical Outcomes
Session Information
Session Name: Biomarkers: Clinical Outcomes
Session Type: Poster Abstract
Date: Tuesday, June 7, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Serum creatinine, while an insensitive biomarker of allograft injury, is the current standard for assessing the stability of allograft function and guiding kidney transplant management. Recent studies have demonstrated that clinically stable adults frequently have subclinical alloimmune injury that negatively impacts long-term outcomes. We sought to ascertain whether this finding held in a cohort of young adult recipients under 40 years of age compared to a contemporaneous cohort over 40 years of age.
*Methods: We previously conducted a single-center retrospective cohort study of 441 consecutive kidney transplant recipients with 6-month surveillance biopsies. Here, we focused on a subgroup of kidney recipients between 18-40 years of age. The primary exposure was subclinical acute rejection (SCAR), defined as Banff 2019 borderline changes, T cell-mediated rejection, or antibody-mediated rejection in a 6-month surveillance biopsy. The primary endpoint was a 3-year composite of clinical acute rejection (CR) or graft failure after surveillance. Secondary exposures included subgroups with isolated SCAR, isolated CR, or both SCAR and CR.
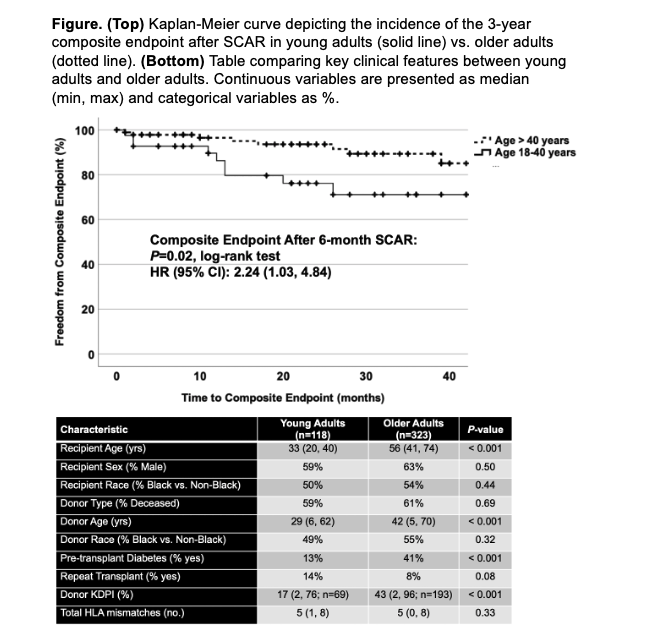
*Results: We analyzed 118 young adult kidney transplant recipients with clinical follow-up right-censored at 40 months post-transplant and compared them to a contemporaneous subgroup of older adult kidney recipients (n=323). The two cohorts had modest but expected clinical and demographic differences (Figure). SCAR was detected in 16% of young adults and 14% of older adults (P=NS); 56% of SCAR cases were the subclinical borderline phenotype. Compared to those with a normal 6-month surveillance biopsy, SCAR was associated with an increased incidence of the 3-year composite endpoint in young adults (42% vs. 15%; P=0.007), including more CR (32% vs. 12%; P=0.03) and death-censored allograft failure (37% vs. 6%; P<0.001). Compared to the older adult cohort, young adults with SCAR had a greater incidence of the composite endpoint (Figure).
*Conclusions: As with older adults, SCAR at 6 months post-transplant in young adults had a significant negative impact on late acute rejection rates and graft survival. The magnitude of impact was greater in young adults despite an expectation for better outcomes based on donor and recipient characteristics. We speculate this may relate in part to poorer medication adherence or more robust alloimmune responses in young versus older adults.
To cite this abstract in AMA style:
Raza S, Agarwal G, Fatima H, Gaston R, Hauptfeld-Dolesjek V, Julian B, Kew C, Kumar V, Mehta S, Ong S, Rosenblum F, Towns G, Mannon R, Seifert M. Differential Impact of Subclinical Kidney Transplant Rejection in Young Adults [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/differential-impact-of-subclinical-kidney-transplant-rejection-in-young-adults/. Accessed March 2, 2026.« Back to 2022 American Transplant Congress