Could Intravenous Iron Strengthen The Chances Of Heart Transplantation For Patients With Left Ventricular Assist Devices?
1Department of Pharmacy, Palmetto Health, Columbia, SC, 2Clinical Pharmacy and Outcomes Sciences, University of South Carolina, Columbia, SC, 3Cardiothoracic Surgery, Palmetto Health, Columbia, SC, 4Cardiology, Palmetto Health, Columbia, SC
Meeting: 2019 American Transplant Congress
Abstract number: B90
Keywords: Heart transplant patients, Sensitization, Ventricular assist devices
Session Information
Session Name: Poster Session B: Heart and VADs: All Topics
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
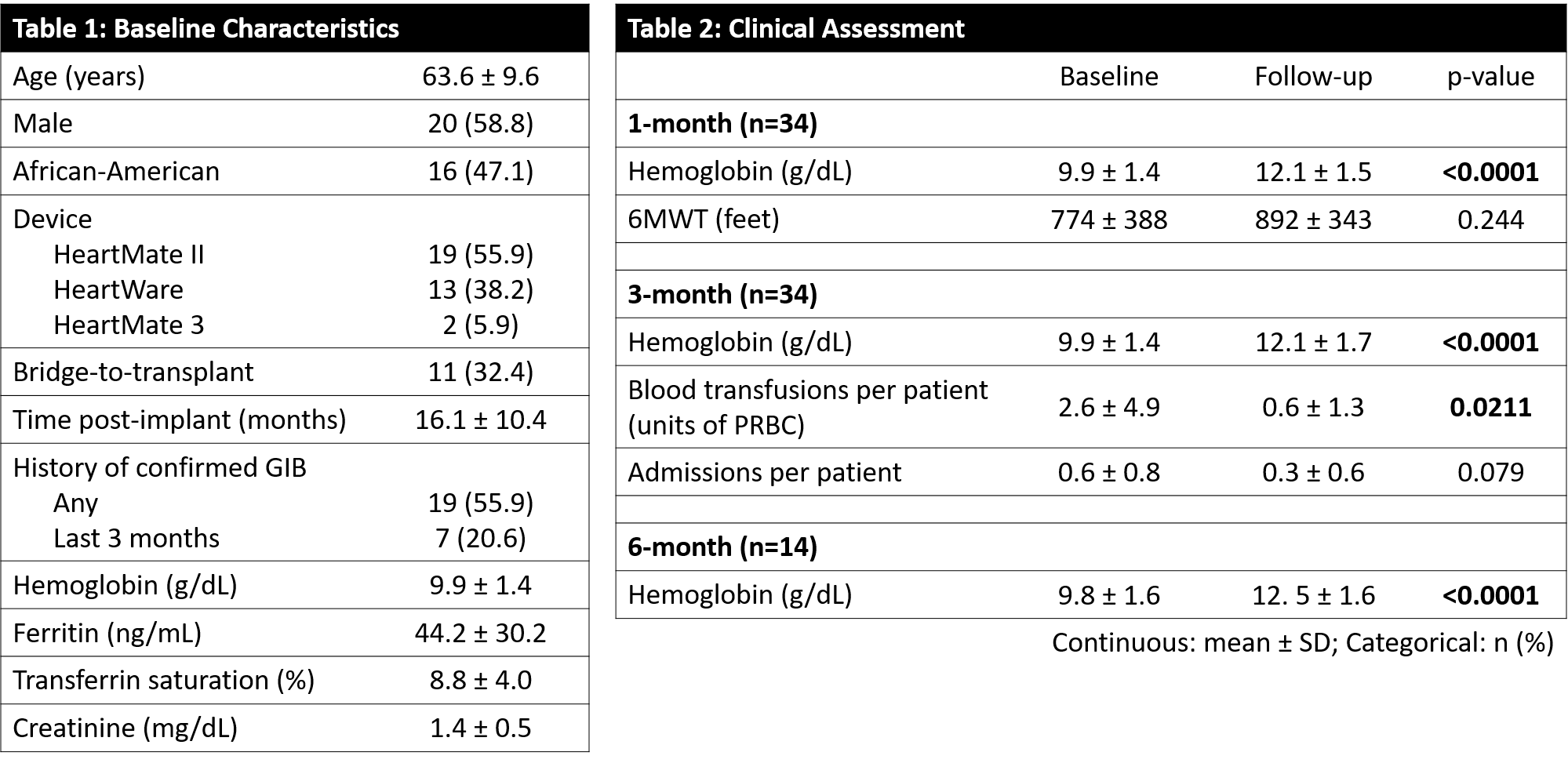
*Purpose: Iron deficiency anemia (IDA) is prevalent in patients supported by left ventricular assist devices (LVADs), is associated with functional limitations, and often warrants blood transfusions. Immunologic sensitization secondary to blood transfusions may lead to delays in transplantation. This pilot study aimed to determine the impact of ferric carboxymaltose (FCM) on IDA, transfusion requirements, readmissions, & functional capacity in an LVAD population.
*Methods: This was a single-center prospective, observational study of LVAD patients at a non-transplant center with IDA (ferritin <100 ng/mL or 100-300 ng/mL with transferrin saturation <20%). Patients received FCM 750 mg x 2 doses as an outpatient. Functional capacity was evaluated by 6-minute walk test (6MWT) prior to and following therapy. Blood transfusion requirements & readmissions were assessed.
*Results: Thirty-four patients received FCM therapy. Baseline data are shown in Table 1. On average, patients were 16 months post-implant, 56% had a history of gastrointestinal bleed (GIB), a third were bridge-to-transplant (BTT), and average baseline lab values included Hgb of 9.9 g/dL and ferritin of 44.2 ng/mL. At 1 month, the average Hgb was significantly improved (12.1±1.5 g/dL vs 9.9±1.4, p<0.0001), and this continued at 3 months (12.1±1.7, p<0.0001) and 6 months (12.5±1.6, p<0.0001) post-treatment. Blood transfusion requirements were significantly lower in the 3 months post-therapy versus the prior 3 months, though the reduction in admissions over this period did not reach statistical significance. While all patients noted subjective functional improvements, there was no difference in 6MWT (Table 2).
*Conclusions: Pilot data in this prospective evaluation of IV iron replacement in LVAD patients with IDA shows a significant improvement in Hgb through 6 months with reduced blood transfusion requirements. Future directions include assessing the impact of limiting IDA-related blood transfusions on panel reactive antibody, other markers of functional status, and transplant rate in the BTT population.
To cite this abstract in AMA style:
Mardis A, Mardis C, Barham J, Poole A, Branham S, Napier R, Martin J, McCann P. Could Intravenous Iron Strengthen The Chances Of Heart Transplantation For Patients With Left Ventricular Assist Devices? [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/could-intravenous-iron-strengthen-the-chances-of-heart-transplantation-for-patients-with-left-ventricular-assist-devices/. Accessed February 23, 2026.« Back to 2019 American Transplant Congress