Correlations between Preoperative Hepatic Venous Pressure Gradient and Graft Hemodynamics after Reperfusion in Living Donor Liver Transplantation
H. Matsushima, M. Fujiki, K. Sasaki, F. Aucejo, T. Diago Uso, C. Kwon, B. Eghtesad, C. Miller, C. Quintini, K. Hashimoto
General Surgery, Digestive Disease & Surgery Institute, Cleveland Clinic, Cleveland Clinic, Cleveland, OH
Meeting: 2019 American Transplant Congress
Abstract number: B350
Keywords: Liver transplantation, Living-related liver donors
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Hepatic venous pressure gradient (HVPG) is known to correlate with severity of portal hypertension in patients with liver cirrhosis. We retrospectively investigated the clinical significance of preoperative HVPG and its correlations with graft hemodynamics after reperfusion in living donor liver transplantation (LDLT).
*Methods: Seventy-five patients who underwent adult-to-adult LDLT at our institution were divided into two groups according to HVPG using a cutoff value of 16 mmHg as previously reported. We investigated the correlations between preoperative HVPG and patient characteristics, surgical outcomes, and post-reperfusion graft hemodynamics including intraoperative portal vein flow (PVF) and hepatic artery flow (HAF).
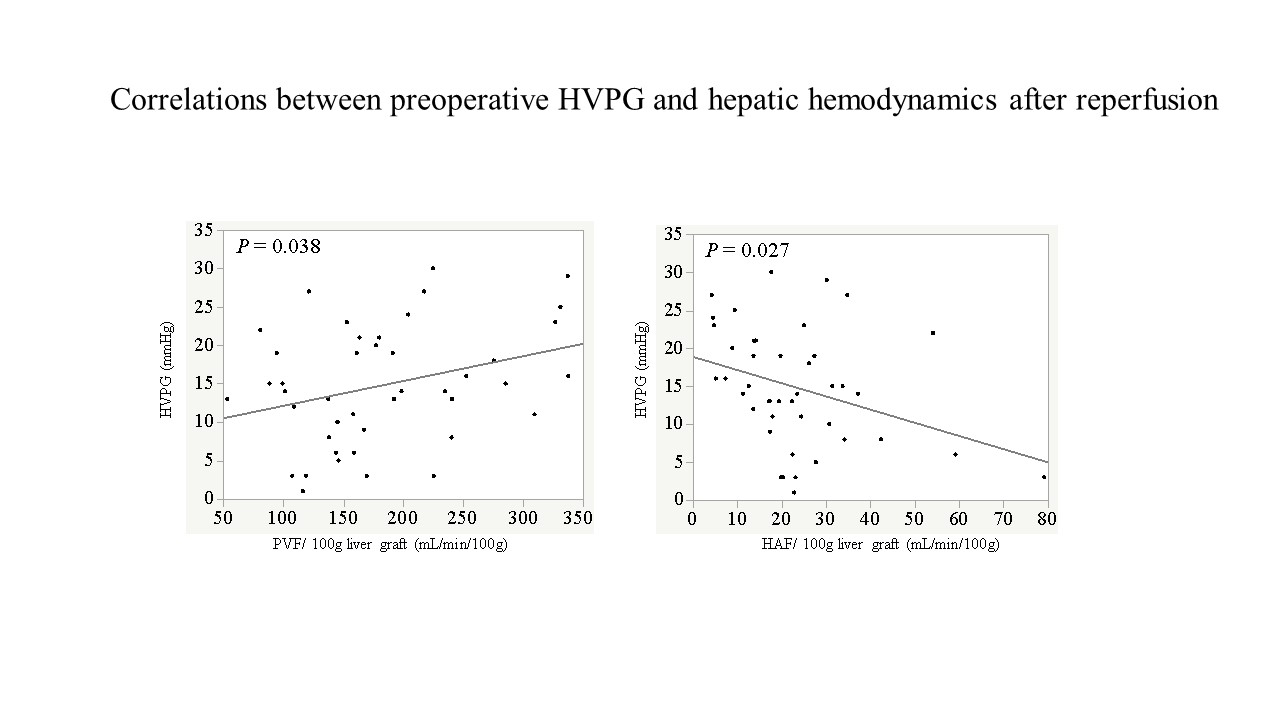
*Results: Thirty-five patients (46.7%) had an HVPG > 16 mmHg. These patients had significantly higher international normalized ratios (INR) and creatinine levels compared to the 40 patients with HVPG < 16 mmHg. They also had higher rates of encephalopathy and intractable ascites, and lower platelet counts compared to those with HVPG < 16 mmHg. Portal inflow modulation was frequently performed in the patients with HVPG > 16 mmHg compared to those with HVPG < 16 mmHg. No significant differences were found in surgical outcomes after LDLT between these two groups, except for postoperative ascites. Preoperative HVPG showed a positive correlation with PVF and a negative correlation with HAF after graft reperfusion (p = 0.038 and p = 0.027, respectively). In linear regression analyses, preoperative HVPG was independently associated with PVF after graft reperfusion.
*Conclusions: Preoperative HVPG was associated with hepatic hemodynamics after graft implantation in LDLT. HVPG as a routine preoperative evaluation may be helpful for surgical planning of portal inflow modulation.
To cite this abstract in AMA style:
Matsushima H, Fujiki M, Sasaki K, Aucejo F, Uso TDiago, Kwon C, Eghtesad B, Miller C, Quintini C, Hashimoto K. Correlations between Preoperative Hepatic Venous Pressure Gradient and Graft Hemodynamics after Reperfusion in Living Donor Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/correlations-between-preoperative-hepatic-venous-pressure-gradient-and-graft-hemodynamics-after-reperfusion-in-living-donor-liver-transplantation/. Accessed June 30, 2025.« Back to 2019 American Transplant Congress