Consequences of Being Listed at a Small Pancreas Program
1Surgery, University of Maryland, Baltimore, MD
2UNOS, Richmond, VA
3Surgery, Indiana University, Indianapolis, IN
4Surgery, University of Wisconsin, Madison, WI.
Meeting: 2018 American Transplant Congress
Abstract number: 371
Keywords: Allocation, Graft failure, Pancreas, Waiting lists
Session Information
Session Name: Concurrent Session: Pancreas and Islet - 1
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:30pm-4:42pm
Presentation Time: 4:30pm-4:42pm
Location: Room 4C-3
How pancreas transplant center (PTC) volume affects patient outcomes after listing is unclear. Low volumes may lengthen waiting times or limit access to transplantation. We examined patient outcomes at large, medium, and small volume PTCs, including waitlist outcomes, and patient disposition if a PTC is inactivated.
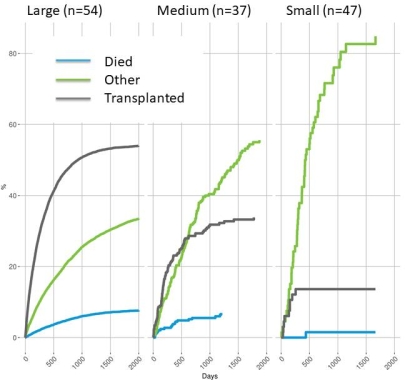
PTCs were grouped by yearly transplant volume: large (n=54): >4, medium (n=37): 2-4, and small (n=47): <2. Outcomes of waitlisted and transplanted pancreas alone (PA) and kidney-pancreas (SPK) candidates from 2010-2015 were evaluated by survival analyses using UNOS data. Waiting times, waitlist outcomes, patient and pancreas graft survival were compared between PTCs. The disposition of candidates listed at PTCs that were inactivated between 2015-2017 were examined.
8151 SPK and 2616 PA candidates were listed; 4580 SPK and 1213 PA transplants were performed. Median waiting times to transplant were 7.5, 13.2, and 15.7 months at large, medium, and small PTCs, respectively. Over 65.7 months, more patients went on to transplant (54%) at large, compared to medium (44%) or small (21%) PTCs (p<0.0001), (Fig 1), where PTC patients were more often delisted for reasons other than death or transplant (p<0.001). Candidate survival from listing until 2 years thereafter was similar when comparing volume size for SPK (p=0.31), or PA (p=0.27) PTCs. One-year recipient survival was worse for SPK recipients at small v large PTCs (p=0.029, HR 1.46 (CI=1.04-2.06)), but not for PA recipients (p=0.92). One-year pancreas graft failure was higher in SPK (HR 1.69, CI=1.24-2.32) and PA recipients (HR 1.74, CI=1.09-2.8) at small v large PTCs. 19 PTCs were inactivated. Only 46 of 146 affected candidates were re-listed: 21 of 39 were transplanted at large PTCs; 2 of 7 were transplanted at medium/small PTCs.
Patients listed for pancreas transplant at large PTCs have shorter waiting times, better waitlist outcomes, and higher one-year patient and pancreas graft survival. Patients re-listed from inactivated PTCs are more likely transplanted at large PTCs.
CITATION INFORMATION: Niederhaus S., Curry M., Fox A., Fridell J., Odorico J. Consequences of Being Listed at a Small Pancreas Program Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Niederhaus S, Curry M, Fox A, Fridell J, Odorico J. Consequences of Being Listed at a Small Pancreas Program [abstract]. https://atcmeetingabstracts.com/abstract/consequences-of-being-listed-at-a-small-pancreas-program/. Accessed March 9, 2026.« Back to 2018 American Transplant Congress