Comparison of Six-Month Outcomes in Patients Bridged to Heart Transplantation with Percutaneous Temporary Circulatory Support Before and after the UNOS Allocation System Change
1Keck Hospital of USC, Los Angeles, CA, 2Newark Beth Israel Medical Center, Newark, NJ, 3Harbor UCLA Medical Center, Los Angeles, CA, 4University of Arizona Sarver Heart Center, Tucson, AZ
Meeting: 2020 American Transplant Congress
Abstract number: B-272
Keywords: Heart/lung transplantation, Mortality, Ventricular assist devices
Session Information
Session Name: Poster Session B: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: We report the trends in utilization and outcomes of percutaneous temporary circulatory support (TCS) in the forms of Impella or TandemHeart as a bridge to heart transplantation (HT) in the six-month period immediately before and after the implementation of the revised United Network of Organ Sharing (UNOS) allocation system in October 2018.
*Methods: The UNOS database was queried for HT candidates who required percutaneous TCS in the forms of Impella or TandemHeart as a bridge to transplant within a 6-month time window before (N=18) and after (N=28) the UNOS allocation change. Comparisons between these cohorts were reported using standard statistical methods and survival analysis was performed using multivariate Cox proportional hazard modeling.
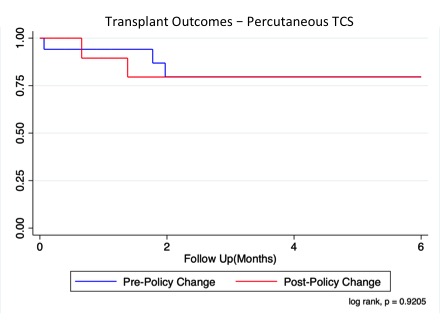
*Results: The absolute number of patients who received percutaneous TCS as a bridge to HT was higher following the UNOS policy change (18 patients vs. 28 patients). No differences were observed in recipient age, diabetes status, donor age or donor organ ischemic time. Furthermore, no differences were observed in utilization of intra-aortic balloon pump or mechanical ventilator support in this population. Waitlist times for patients with percutaneous TCS were significantly shorter following the allocation change (Median [interquartile range], 22.5 [8.0, 84.0] days vs. 6.5 [2.5, 14.5] days, p = 0.001). Of note, no difference in 6-month survival was observed in patients bridged to HT with percutaneous TCS before and after the UNOS allocation change (p = 0.9205).
*Conclusions: The number of HT candidates on percutaneous TCS at the time of HT has increased following implementation of the new UNOS allocation system with a concurrent reduction in candidate waitlist time, but no difference in post-HT mortality. The increased volume of HT for patients with percutaneous TCS and reduction in waitlist times reflects a successful effort to restratify the large pool of previously status 1A candidates in a way that provides more granularity to the waitlist hierarchy.
To cite this abstract in AMA style:
Nattiv J, Liu GS, Banankhah P, Sussex J, Genyk P, Li J, Vucicevic D, Chand RS, Pandya K, Rahman J, Wolfson AM, Vaidya AS, DePasquale E. Comparison of Six-Month Outcomes in Patients Bridged to Heart Transplantation with Percutaneous Temporary Circulatory Support Before and after the UNOS Allocation System Change [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/comparison-of-six-month-outcomes-in-patients-bridged-to-heart-transplantation-with-percutaneous-temporary-circulatory-support-before-and-after-the-unos-allocation-system-change/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress