Comparable Outcomes of Deceased Donor Liver Transplant Outcomes in Recipients with Previous Abdominal Surgery (PAS) after Pre Listing Surgical Categorization. A Propensity-Score Matched Pair Analysis
Department of Transplant Surgery, Ochsner Medical Center, New Orleans, LA
Meeting: 2019 American Transplant Congress
Abstract number: A305
Keywords: Graft survival, Liver transplantation, Safety
Session Information
Session Name: Poster Session A: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Few studies have evaluated the impact of previous abdominal surgery (PAS) on deceased donor liver transplantation-(DDLT). Furthermore, there is no evidence of impact of pre-LT surgical-risk-categorization on recipients with PAS. We evaluated the outcomes of liver-transplantation in patients with PAS and surgical-risk-categorization.
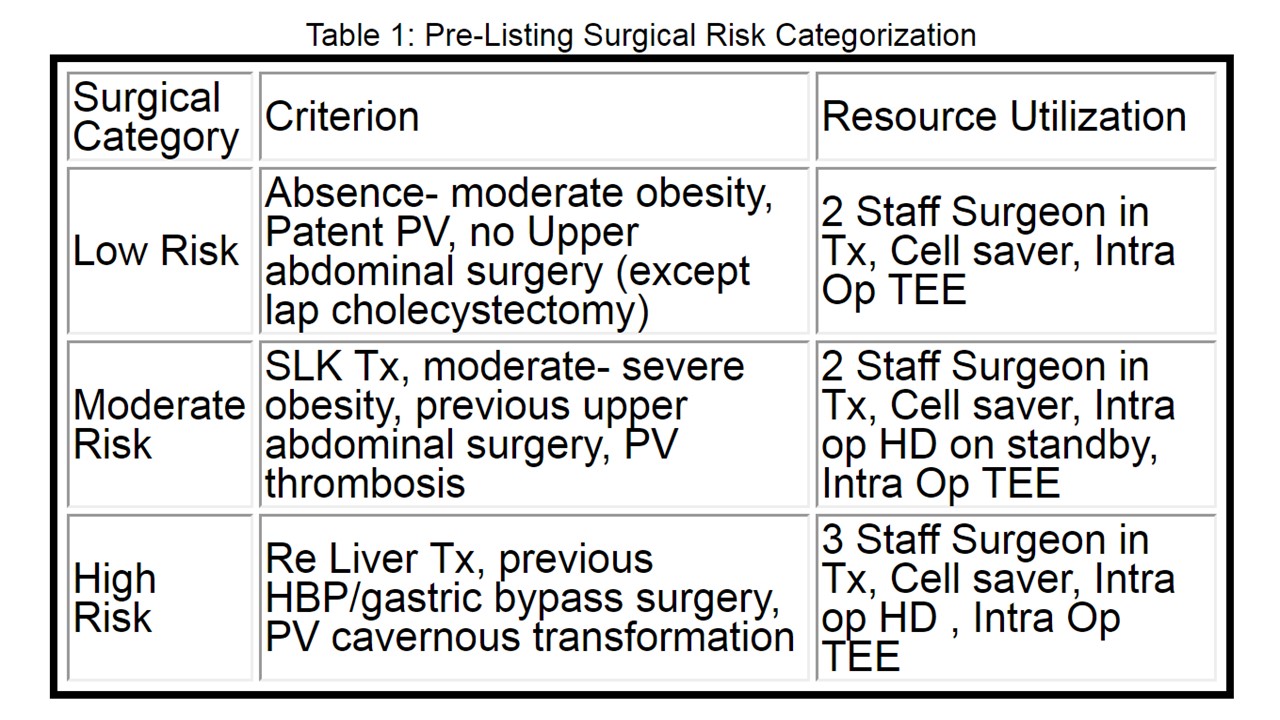
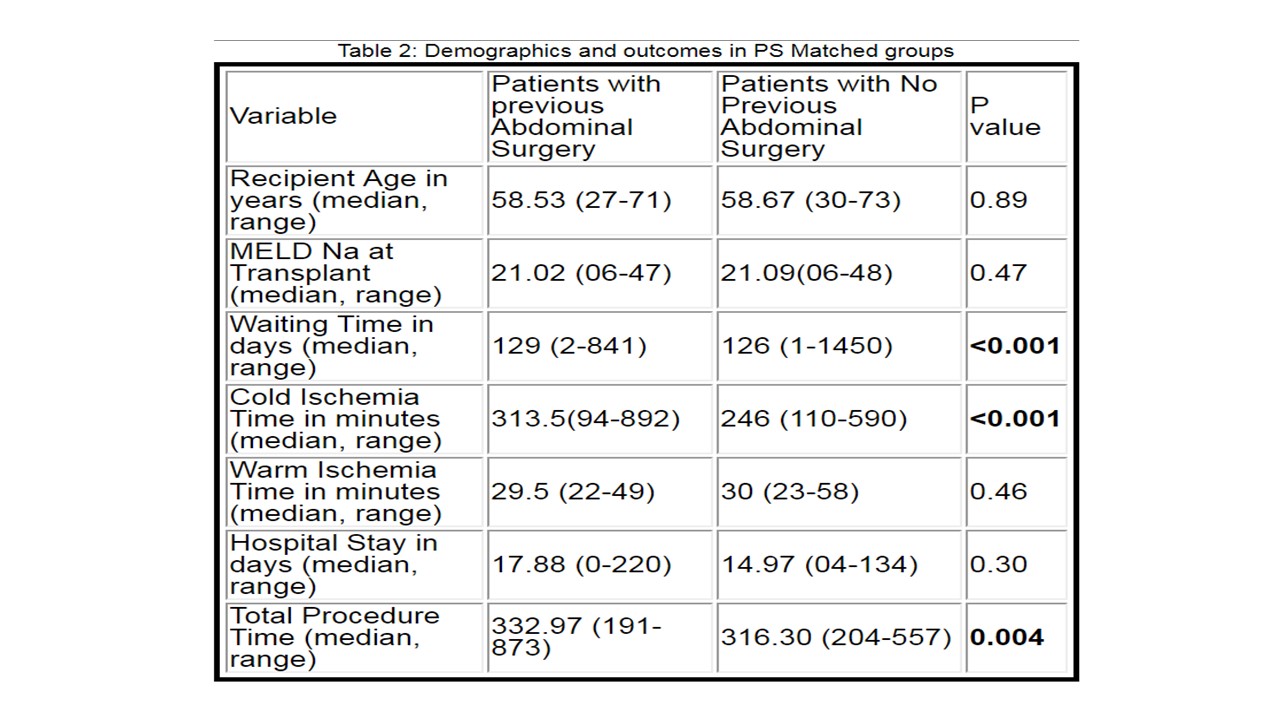
*Methods: Our Institution has been assigning the potential recipient with surgical-complexity-category since 2014 to preempt surgical-risk (Table 1) and optimize resource-utilization for complex-cases. Outcome data from all N=485 DDLT-recipients (N=235 with PAS, N=250 with no PAS) operated between Jan-15 and June-17 were compared. The primary-endpoint of the study was patient-survival and graft-survival at 30 d, 180 d and 1 year. As secondary-outcomes, hospital-stay, waiting-time, early-allo-graft-dysfunction, biliary-complications, hepatic-artery-stenosis/thrombosis, portal-vein-thrombosis, re-exploration rates were compared. Propensity-score (PS) estimation with nearest-neighbor-matching, controlling for donor/recipient age; BMI and DRI, matched N=168 PAS & N=168 non-PAS-recipients. Multivariate-analysis for Patient/Graft-Survival was performed using the Cox-proportional-hazards-model.
*Results: There were no significant differences in Graft/Patient survival in PAS/no PAS matched cohorts at 30 d, 180 d and 1 year (Fig-1). Recipients with PAS had higher-median-waiting-time, Cold-ischemia-time and Total-procedure-time. (Table-2). 92% recipients in PAS-cohort had DBD-DDLT v/s 71% in no-PAS-cohort (p=0.003). There were no statistical-differences in Early-Allograft-Dysfunction-rate OR-1.31(0.78-2.19); Biliary-complication-rate OR-1.26(0.79-2.01); Hepatic-Artery-Stenosis-rate OR-1.37(0.73-2.58); Hepatic-Artery-thrombosis-rate OR-1.33(0.35-5.01); Portal-vein-thrombosis-rate OR-1.07(0.51-2.23) and Re-Exploration-rate OR-1.25(0.64-2.45). DDLT-PAS-cohort had higher intra-op-RBC >5-units OR-1.04(1.02- 1.07) and AKI OR-1.51(1.02-2.24). On sub group analysis of no PAS v/s Lower (LAS) and Upper (UAS) abdominal surgery.,UAS had higher intra-operative RBC transfusion rate and Operative Time(p<0.001) compared to no PAS cohort. Results were similar between no-PAS and LAS group (p=NS). On sub-sub group analysis of UAS cohort ; Re Transplant, hepatobiliary, bariatric surgeries cohort had higher RBC transfusion rate, longer OT and hospital stay compared to lap cholecystectomy. (p<0.001)
*Conclusions: PAS impacts the LT procedure yet granular analysis suggests that complicated UAS has higher risk of inferior outcomes than straightforward lap cholecystectomies and LAS. By using pre-listing surgical categorization and resource management, we were able to achieve equitable results with complex transplants..
To cite this abstract in AMA style:
Sharma H, Bohorquez H, Oganesyan D, Bruce D, Bugeaud E, Carmody I, Cohen A, Seal J, Sonnier D, Loss G. Comparable Outcomes of Deceased Donor Liver Transplant Outcomes in Recipients with Previous Abdominal Surgery (PAS) after Pre Listing Surgical Categorization. A Propensity-Score Matched Pair Analysis [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/comparable-outcomes-of-deceased-donor-liver-transplant-outcomes-in-recipients-with-previous-abdominal-surgery-pas-after-pre-listing-surgical-categorization-a-propensity-score-matched-pair-analysis/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress