Combined Heart-Liver Transplantation: A Systematic Review of the Literature
1Vanderbilt University Medical Center, Nashville, TN, 2Society of Junior Doctors, Athens, Greece, 3Aristotle University of Thessaloniki, Thessaloniki, Greece
Meeting: 2020 American Transplant Congress
Abstract number: C-285
Keywords: Heart, Heart transplant patients, Liver transplantation, Outcome
Session Information
Session Name: Poster Session C: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Combined heart-liver transplant (CHLT) has been increasingly utilized as the treatment of choice for candidates with dual end-stage organ disease. We aimed to assess the indications, surgical practices and outcomes of CHLT worldwide.
*Methods: We performed a systematic literature review of the PubMed and Scopus databases (end-of-search date: June 22nd, 2019) with respect to the PRISMA statement.
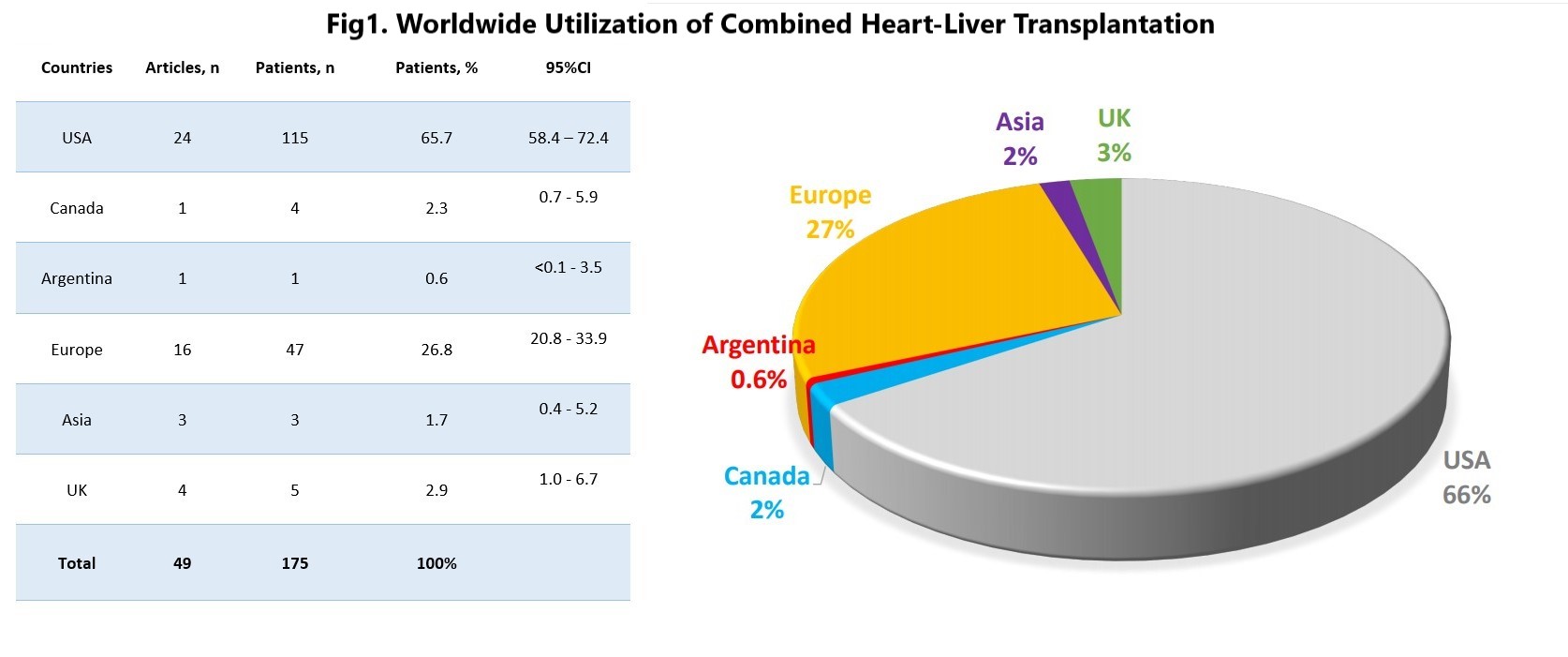
*Results: The search yielded 49 eligible case reports/series, reporting on a total of 175 patients undergoing CHLT (Fig1). Mean patient age was 44.2±13.8 years and 62.7% were male. The indications for transplantation were amyloidosis in 36% (n=63/175; 95%CI: 29.3-43.4), cardiomyopathy in 29.1% (n=51/175; 95%CI: 22.9-36.3), congenital heart disease in 24% (n=42/175; 95%CI: 18.3-30.9), and unknown in 10.9% (n=19/175; 95%CI: 7.0-16.4). Synchronous transplantation (CHLT at the same operation) was performed in 88% (n=154/175; 95%CI: 82.3-92.1), with 74% (n=114/154; 95%CI: 66.6-80.3) being HT first, 7.1% en-block method (n=11/154; 95%CI: 3.9-12.5) and 1.3% LT first (n=2/154; 95%CI: 0.06-4.9). Sequential transplantation (on different dates) was reported in 9.1% (n=16/175; 95%CI: 5.6-14.4), with HT performed before LT in 62.5% (n=10/16; 95%CI: 38.5-81.6) and LT performed before HT in 12.5% (n=2/16; 95%CI: 2.2-37.3). Mean MELD score was 15.6±5.6 at listing, and 13.9±6.6 at transplant, while the mean Child-Pugh score was 8.2±1.8. The mean ejection fraction pre- and post-operatively was 44.5±18.1 and 61.2±4.7, respectively. Total operation time was 818±183 min, donor heart ischemic time was 195±62 min, cardiopulmonary bypass time was 208±81 min, heart cold ischemia time (CIT) was 208±74 min, and liver CIT was 445±150 min. Overall survival rate at 30 days was 95.2% (n=157/165; 95%CI: 90.6-97.7), at 6 months 90.4% (n=113/125; 95%CI: 83.8-94.6), at 1 year 86.7% (n=104/120; 95%CI: 79.3-91.7), at 3 years 74.7% (n=68/91; 95%CI: 64.9-82.6), and at 5 years 65.8% (n=48/73; 95%CI: 54.3-75.6).
*Conclusions: This study highlights the feasibility of CHLT in appropriately selected patients with coexisting heart and liver disease in high-volume transplant centers. With more than 65% 5-year survival, CHLT should be considered as a reasonable treatment option for patients with dual organ failure.
To cite this abstract in AMA style:
Ziogas IA, Giannis D, Kapsampelis P, Giannopoulou A, Evangeliou A, Mylonas KS, Tsoulfas G, Matsuoka LK, Montenovo MI, Izzy M, Alexopoulos SP. Combined Heart-Liver Transplantation: A Systematic Review of the Literature [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/combined-heart-liver-transplantation-a-systematic-review-of-the-literature/. Accessed February 23, 2026.« Back to 2020 American Transplant Congress