CMV-Specific Cell-Mediated Immunity after Valgancyclovir Prophylaxis Predicts Late Onset CMV Infection in Kidney Transplant Patients
1Experimental Nephrology Laboratory, IDIBELL, Barcelona, Spain
2Nephrology Department, Bellvitge University Hospital, Barcelona, Spain.
Meeting: 2018 American Transplant Congress
Abstract number: 184
Keywords: Cytomeglovirus, Kidney transplantation, Monitoring, T cell reactivity
Session Information
Session Name: Concurrent Session: CMV: Bench to Bedside
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: Room 608/609
Background: There is currently no means to predict late-onset CMV infection after a long course of post-transplant Valgancyclovir prophylaxis therapy and its development still negatively impacts on graft and patient outcomes. However, CMV-sp CMI has shown promise to identify at-risk patients of developing CMV infection after transplantation.
Methods: 89 consecutive R+ KT patients were evaluated at the time of Valgancyclovir prophylaxis withdrawal for their CMV-sp CMI against main antigens (IE-1, pp65) using the T-SPOT.CMV®, to predict late onset infection.
Results: 49/89 (44.9%) received anti-ILR2A and 40/89 (55.1%) rATG induction therapy. All patients received a TAC/MMF-based immunosuppression. 10/89 (11.2%) patients developed late onset CMV infection. When all patients were pooled together, CMV-sp CMI to IE-1 and pp65 were significantly lower in patients displaying CMV infection than those that did not (48.3±73.7 vs 195.3±224.8, p<0.001 for IE-1 and 164.7±192.3 vs 338.4±263.3 IFN-γ spots, p=0.047 for pp65). CMV-sp CMI was significantly lower in patients developing CMV infection when stratifying according to the type of induction therapy either anti-IL2RA or rATG. A ROC curve analysis was performed in order to stablish the most sensitive and specific CMI cut-off to classify patients into High(HR), Intermediate(IR) and low(LR) risk. Cumulative incidence of CMV infection among HR was significantly higher than IR and LR (Log-rank<0.001) (HR 9.09, 95%CI 2.34-35.19, p=0.001). 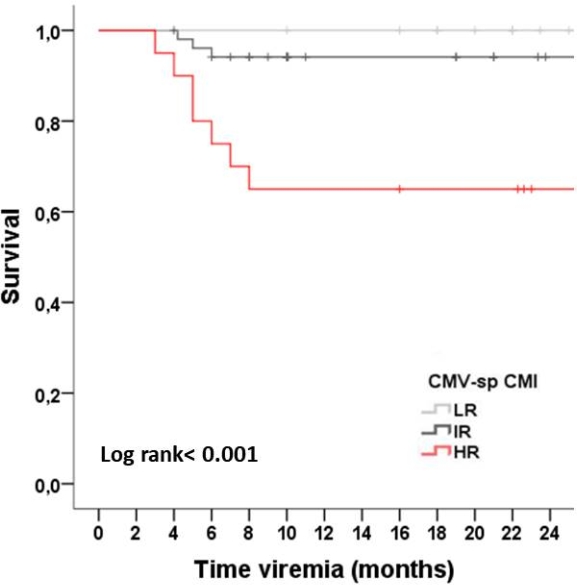 Sensitivity, specificity, PPV and NPV of CMV-sp CMI predicting CMV infection was 70%, 83.5%, 35%, 95.7%, respectively.
Sensitivity, specificity, PPV and NPV of CMV-sp CMI predicting CMV infection was 70%, 83.5%, 35%, 95.7%, respectively.
Conclusions: Monitoring CMV-sp CMI after valgancyclovir prophylaxis withdrawal is able to accurately rule out KT at high risk of late-onset CMV infection, regardless other traditional clinical variables.
CITATION INFORMATION: Jarque M., Crespo E., Melilli E., Manonelles A., Montero N., Luque S., Cruzado J., Grinyo J., Bestard O. CMV-Specific Cell-Mediated Immunity after Valgancyclovir Prophylaxis Predicts Late Onset CMV Infection in Kidney Transplant Patients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Jarque M, Crespo E, Melilli E, Manonelles A, Montero N, Luque S, Cruzado J, Grinyo J, Bestard O. CMV-Specific Cell-Mediated Immunity after Valgancyclovir Prophylaxis Predicts Late Onset CMV Infection in Kidney Transplant Patients [abstract]. https://atcmeetingabstracts.com/abstract/cmv-specific-cell-mediated-immunity-after-valgancyclovir-prophylaxis-predicts-late-onset-cmv-infection-in-kidney-transplant-patients/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress
