Clinical Stratification of Pediatric Liver Transplant Recipients 4-5 Years Post-Transplant: 1St Step Towards Personalized Management
1University of California, San Francisco, San Francisco, CA, 2Mount Sinai Kravis Children's Hospital and Recanati/Miller Transplantation Institute, Mount Sinai Health System, New York, NY
Meeting: 2022 American Transplant Congress
Abstract number: 1447
Keywords: Biopsy, Immunosuppression, Liver transplantation, Monitoring
Topic: Clinical Science » Liver » 61 - Liver: Pediatrics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Recent surveillance biopsy studies strongly associate high normal ALT (>35U/L) with inflammatory histopathology and low normal ALT (<15U/L) with its absence, suggesting that ALT can inform decision-making regarding immunosuppression (IS) dosing and/or biopsy1,2. We aim to map liver transplant (LT) recipients by a single ALT metric for the 1-year period starting 4 years after LT to show the distribution of ALT for a pediatric population.
*Methods: Data on 97 children transplanted 2005-2016 with ≥1 ALT during the 5th year after LT were extracted and analyzed. We first calculated the median ALT/AST for each month of the year. The medians were then used to calculate the mean ALT/AST for the year. Univariable analysis identified associations between mean ALT and multiple clinical variables including tacrolimus standard deviation (SD), which was calculated when ≥3 tacrolimus levels were available.
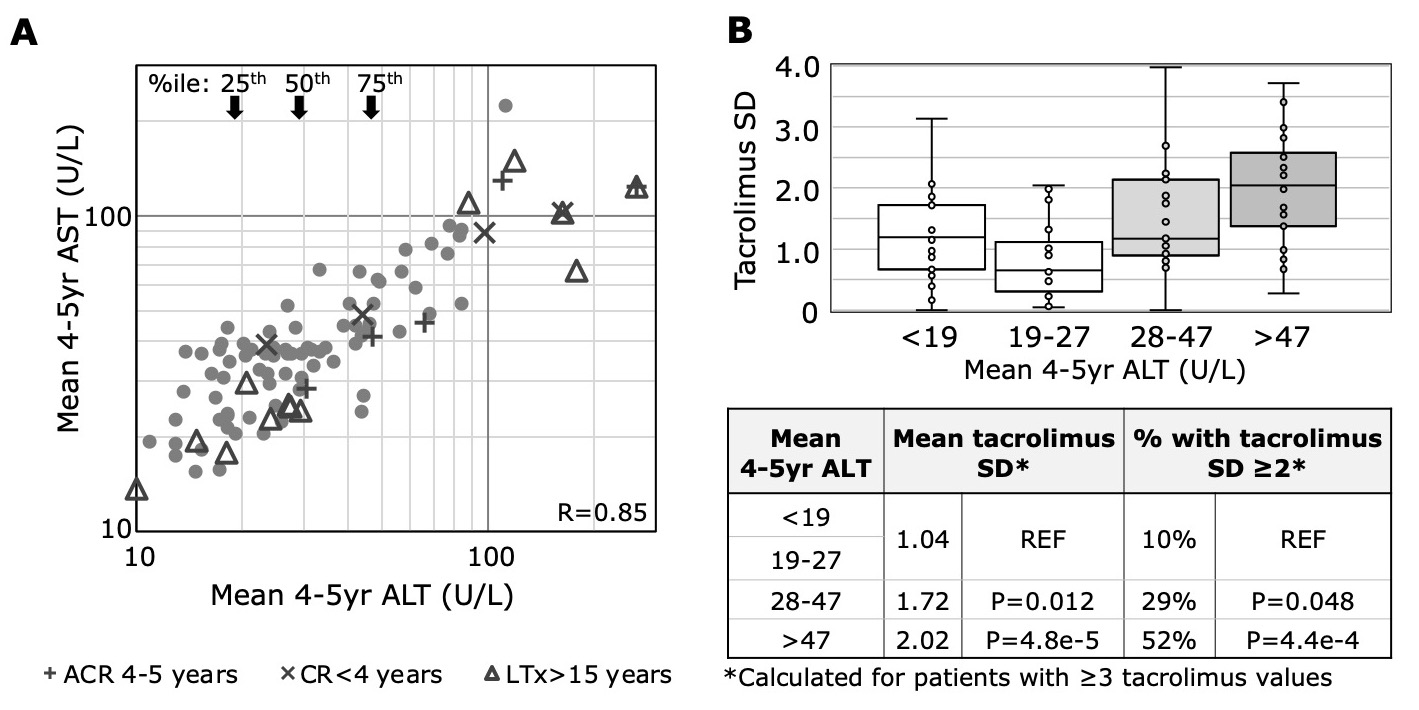
*Results: For our cohort of 97 children [49 male; 77 deceased donors; median (IQR) age at LT of 2.47 (10.9) yrs], the 25th, 50th, and 75th %iles for mean 4-5yr ALT/AST (U/L) were 19/26, 28/36, 47/49, respectively (Fig 1A). ALT correlated strongly with AST (R=0.85). Variables associated with high mean 4-5yr ALT include age at LT >15yrs (n=13; p=0.0006), chronic rejection (CR) diagnosis prior to yr4 (n=4; p=0.03), and acute cellular rejection (ACR) episode in yr4-5 (n=5; p=0.0001). Sex, donor type, LT indication, retransplant within 30 days, and ACR history were not correlated. Compared to children with ALT<28 (1st, 2nd quartiles combined), those with ALT 28-47 (3rd) or >47 (4th) had significantly higher tacrolimus SDs [1.04 vs. 1.72 (3rd) and 2.02 (4th)] and higher % with tacrolimus SD≥2 [10% vs. 29% (3rd) and 52% (4th)] (Figure 1B). Mean tacrolimus levels did not significantly differ between the ALT quartiles.
*Conclusions: Among children with LTs, 50% have low mean 4-5yr ALT and low tacrolimus SD, and thus perhaps are prime candidates for IS minimization. For the remaining 50% with moderate or high mean 4-5yr ALT, additional metrics such as tacrolimus SD and/or donor specific antibody1,2 may further risk stratify to motivate implementation of adherence measures, liver biopsy and/or IS escalation. Nuanced consideration of readily available, non-invasive data may facilitate safe and personalized IS dosing and reduce the frequency of allograft biopsy. (1Vionnet, JHep 2021; 2Feng, Gastro 2018)
To cite this abstract in AMA style:
Dixon W, Perito ER, Tavakol M, Bucuvalas J, Feng S. Clinical Stratification of Pediatric Liver Transplant Recipients 4-5 Years Post-Transplant: 1St Step Towards Personalized Management [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/clinical-stratification-of-pediatric-liver-transplant-recipients-4-5-years-post-transplant-1st-step-towards-personalized-management/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress